The tenth edition of the International Classification of Diseases (ICD-10) (World Health Organization, 1992) advanced the study of remitting psychoses with acute onset by proposing the tentative diagnoses of acute and transient psychotic disorders (ATPD). These include four specific and two non-specific disorders (Table 1). Despite some early attempts to validate these diagnoses (Reference Jørgensen, Bennedsen and ChristensenJørgensen et al, 1997; Reference Malhotra, Varma and MisraMalhotra et al, 1998), their boundaries remain elusive. Results of studies by our group suggested that remitting psychoses with acute onset typically last longer than the maximum 1-3 months allowed for ATPD, and that the duration might be different between developing and industrialised settings (Susser et al, Reference Susser, Fenning and Jandorf1995a ,Reference Susser, Varma and Malhotra b ). Following this, the present study examines the duration and the use of ATPD criteria across settings in a large international sample in which we previously delineated remitting psychoses with acute onset from schizophrenia through their distinct epidemiological characteristics (Reference Susser and WanderlingSusser & Wanderling, 1994).
Table 1 Sub-classification of acute and transient psychotic disorders (F23) in ICD-10

| Categories | Duration |
|---|---|
| Specific categories | |
| Acute polymorphic psychotic disorder without symptoms of schizophrenia (F23.0) | <3 months |
| Acute polymorphic psychotic disorder with symptoms of schizophrenia (F23.1) | <1 month |
| Acute schizophrenia-like psychotic disorder (F23.2) | <1 month |
| Other acute predominantly delusional psychotic disorders (F23.3) | <3 months |
| Non-specific categories | |
| Other acute and transient psychotic disorders (F23.8) | Not specified |
| Acute and transient psychotic disorder, unspecified (F23.9) | Not specified |
METHOD
The methods of the Determinants of Outcome of Severe Mental Disorders (DOSMeD) study are described elsewhere (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). Briefly in defined catchment areas in 13 sites, investigators were to include all first-contact patients presenting with a psychotic disorder to a helping agency over a 2-year period. Patients ranged in age from 15 to 54 years.
The 13 sites were classified by the original investigators of the DOSMeD into five developing and eight industrialised country sites (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). Developing country sites included Agra, India; Cali, Colombia; urban Chandigarh, India; rural Chandigarh, India; and Ibadan, Nigeria. The industrialised country sites included Aarhus, Denmark; Dublin, Ireland; Honolulu, Hawaii; Moscow, Russia; Nagasaki, Japan; Nottingham, England; Prague, the Czech Republic; and Rochester, NY, USA. In 8 of the 13 sites, the coverage of the catchment area was more comprehensive, and the sample of patients from these sites was considered an incidence cohort (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). These eight sites included two developing country sites (rural Chandigarh and urban Chandigarh) and six industrialized country sites (Aarhus, Dublin, Honolulu, Moscow, Nagasaki, and Nottingham). Note that both developing country incidence sites are in the same region of India; nevertheless, they represent different sociocultural contexts. The rural catchment area in Chandigarh is a green fertile region in Ambala District (Harayan state), which, although more prosperous than many rural Indian locales, has a 56% illiteracy rate. Urban Chandigarh, on the other hand, is one of the more modern cities in India, with a population of about 348 000 in 1980 (Reference Day, Nielsen and KortenDay et al, 1987; Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992; Reference Collins, Varma and WigCollins et al, 1999).
The sample for this study, as in our previous study (Reference Susser and WanderlingSusser & Wanderling, 1994), was drawn from a subset of 794 subjects in the DOSMeD cohort (444 in the eight incidence sites) who met the following inclusion criteria: full intake assessment, completion of a 2-year follow-up, an ICD-9 diagnosis of schizophrenia at study entry, and no clear-cut affective (or other non-psychotic) syndrome during the 2-year follow-up period.
Research instruments
At entry to the study, and at the 2-year follow-up, a research psychiatrist administered the ninth edition of the Present State Examination (PSE; Reference Wing, Cooper and SartoriusWing et al, 1974) and the Diagnostic and Prognostic Schedule (DPS; Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992), and on the basis of these ratings made an ICD-9 diagnosis. In addition, the Psychiatric and Personal History Schedule (PPHS; Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992), usually completed with a key informant, was administered by a mental health professional, often a psychiatric social worker. The interrater reliability for ratings used in the present analyses have been previously reported (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992) and were all well within the acceptable range.
Selection of subjects
For the examination of duration, subjects were selected who had experienced psychosis with acute onset, complete remission and no relapses within the 2-year followup period. These cases are henceforth called remitting psychoses with acute onset. Cases with multiple episodes within the 2-year follow-up period were excluded, because the duration of each individual episode was not recorded in the DOSMeD study.
Onset, course and duration were assessed using specific ratings on the PPHS administered at baseline and at 2-year follow-up. Acute onset (termed ‘sudden onset’ in the PPHS) was operationalised as “a florid psychotic state developed within days (up to a week), without being preceded by any prodromal signs or symptoms”. Complete remission and no relapse was operationalised as “a single psychotic episode followed by a complete remission”, rated at the 2-year follow-up.
Of 794 patients in all 13 sites of the DOSMeD study who had a full initial evaluation, a 2-year follow-up assessment, an ICD-9 schizophrenia diagnosis at study entry, and no clear-cut affective syndrome during the follow-up period, 98 (12%) also met the criteria for remitting psychoses with acute onset as described above. The distribution of cases of remitting psychoses with acute onset according to gender and site is presented in Table 2. Whereas 21% (78 out of 376) of patients in the developing country settings were categorised as cases of remitting psychoses with acute onset, only 5% (20 out of 418) in the industrialised settings could be so categorised.
Table 2 Distribution of remitting psychoses with acute onset according to setting and gender in the Determinants of Outcome of Severe Mental Disorders study

| Centre | No. of females | No. of males | Total no. |
|---|---|---|---|
| Developing country | |||
| Agra | 10 | 16 | 26 |
| Cali | 3 | 5 | 8 |
| Ibadan | 9 | 8 | 17 |
| Chandigarh, urban1 | 11 | 4 | 15 |
| Chandigarh, rural1 | 5 | 7 | 12 |
| Total | 38 | 40 | 78 |
| Industrialised country | |||
| Aarhus1 | 1 | 0 | 1 |
| Moscow1 | 3 | 1 | 4 |
| Honolulu1 | 0 | 0 | 0 |
| Rochester | 0 | 0 | 0 |
| Prague | 6 | 1 | 7 |
| Nagasaki1 | 0 | 1 | 1 |
| Nottingham1 | 4 | 1 | 5 |
| Dublin1 | 1 | 1 | 2 |
| Total | 15 | 5 | 20 |
Examination of duration
Duration of illness was computed as the sum of two ratings made on the PPHS: (a) the duration of illness before intake, rated in months; and (b) the duration of illness during the 2-year follow-up period, rated in weeks (converted to months). We examined the duration of illness in all selected subjects by plotting the duration of illness in 2-month intervals on histograms. First, we examined the distribution in all sites. Next, we examined the distribution of duration in the developing v. industrialised sites separately. Finally, to assess the possibility that the incidence sites might have captured cases with shorter duration which were missed by non-incidence sites, we examined the duration in the eight incidence sites where the ascertainment of cases was more complete.
ICD-10 diagnosis
As part of a 15-year follow-up of the original DOSMeD cohort, psychiatrists at each centre re-diagnosed the patients using ICD-10 criteria (Reference Sartorius, Gulbinat and HarrisonSartorius et al, 1996). For this, they used all available information on each patient. We requested ICD-10 diagnoses from incidence sites for patients with remitting psychoses with acute onset whose illness had lasted 6 months or less. ICD-10 diagnoses for five sites - rural Chandigarh, urban Chandigarh, Nottingham, Dublin and Moscow - are reported here. In two of the incidence sites (Nagasaki and Honolulu), no cases met the inclusion criteria described earlier. The Aarhus site did not take part in the 15-year follow-up study, therefore no ICD-10 diagnoses were available for this centre.
RESULTS
Duration
Figure 1(a) shows the distribution of duration for the 98 cases of remitting psychoses with acute onset in all sites. These cases had a modal duration of 2-4 months with 43% (n=42) of the cases falling within this range. Thirty (31%) cases had a duration of 3 months or less, and only one case (1%) had a duration of 1 month or less.
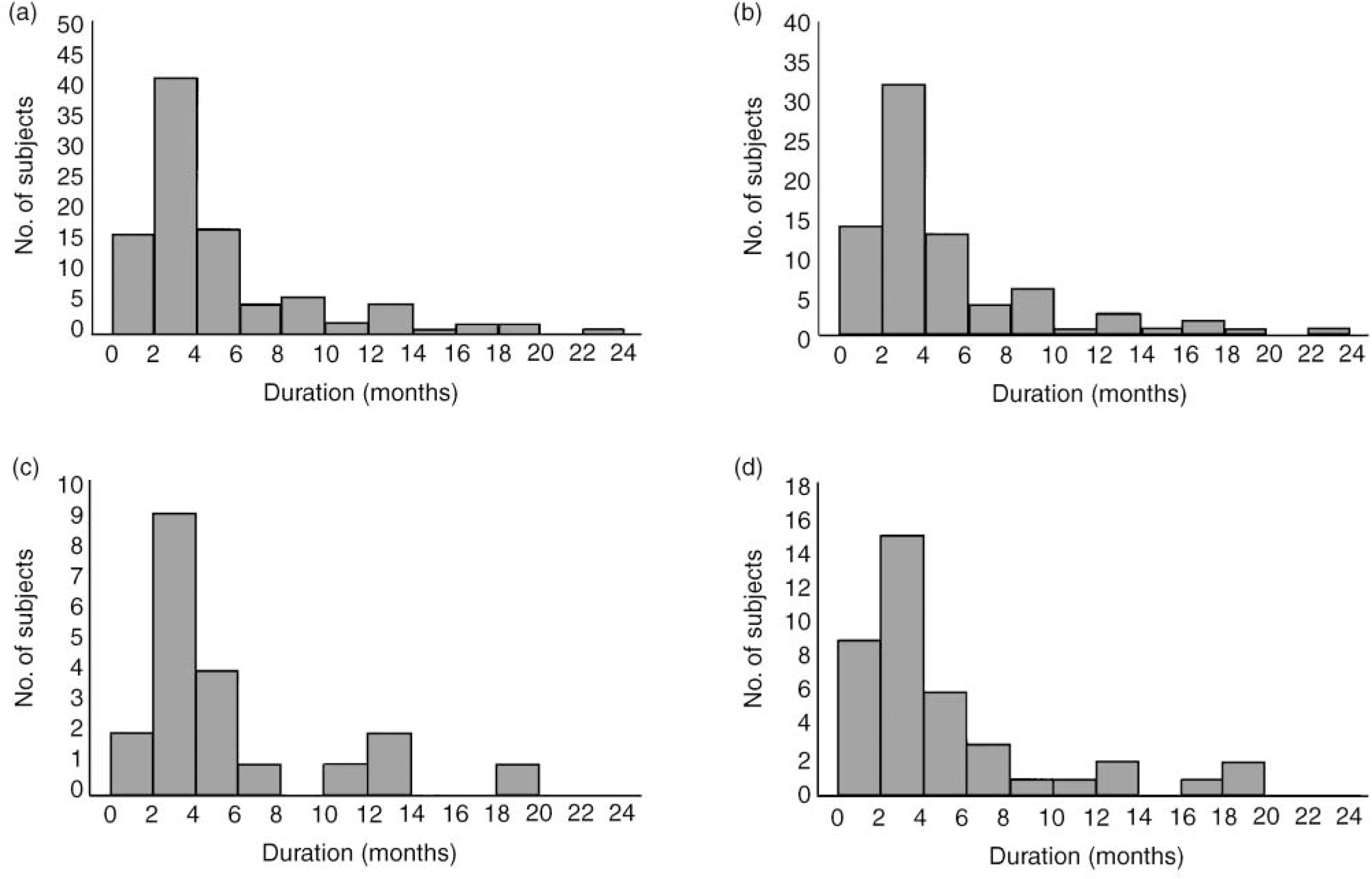
Fig. 1 The distribution of duration of remitting psychoses with acute onset in the Determinants of Outcome of Severe Mental Disorders study for: (a) the 98 cases in all of the 13 sites; (b) the 78 cases in developing country settings; (c) the 20 cases in industrialised country settings; and (d) the 40 cases in the eight incidence sites.
Figures 1(b) and 1(c) show the distribution of duration for the 78 patients from the developing country settings and 20 from the industrialised country settings separately. The pattern was similar across the two settings.
Figure 1(d) shows the distribution of duration for the 40 cases from the eight incidence sites. The pattern was similar to the distribution in all 13 sites.
ICD-10 diagnoses
As noted earlier, we requested ICD-10 diagnoses for patients from incidence sites with remitting psychoses with acute onset, whose illness lasted 6 months or less. Thirty patients in both settings met these criteria. Of these, 10 (33%) were from the industrialised country settings and 20 (67%) from the developing country settings. Eleven (37%) patients were male and 19 (63%) female. ICD-10 diagnoses were available for 27 (90%) of these patients. In the Moscow site, only patients recruited in the first year of the 2 years of the study recruitment were in the 15-year follow-up; as a result two patients from this site did not receive ICD-10 diagnoses. One patient was from the Aarhus site which, as noted earlier, was not included in the follow-up study.
Diagnoses for the 27 cases were as follows: 16 (59%) schizophrenia (F20.0, F20.1, F20.3, F20.5, F20.9); four (15%) other acute and transient psychotic disorder (F23.8); two (7%) acute schizophrenia-like psychotic disorder (F23.2); one (4%) other non-organic psychotic disorder (F28); one (4%) recurrent depressive disorder with psychotic symptoms (F33.3); one (4%) mania with psychotic symptoms (F30.2); one (4%) alcoholic hallucinosis (F10.5); and one (4%) mental and behavioural disorder due to use of other stimulants (F15.5).
DISCUSSION
There were three major findings in this study. The first was that remitting psychoses with acute onset had a modal duration of 2-4 months - longer than the maximum 1-3 months (depending on the specific diagnosis) allowed for the ICD-10 diagnoses of ATPD. Cases from the incidence sites, where ascertainment extended to first contacts with general practitioners and faith healers, had a distribution similar to that of cases from the rest of the DOSMeD sites. Therefore, this finding is unlikely to be explained by a failure to capture the cases with shorter duration.
The second finding was that the distribution of duration was similar between sites classified as ‘developing’ and ‘industrialised’ by the original investigators (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). Earlier findings from different samples had suggested the possibility that remitting psychoses with acute onset might have a longer duration in the developing settings than in the industrialised settings (Susser et al, Reference Susser, Fenning and Jandorf1995a ,Reference Susser, Varma and Malhotra b ). However, these earlier suggestive findings were not corroborated by the present study, which directly compared the duration between the two settings.
The third finding was that only two cases (7%) of the 27 with an ICD-10 diagnosis met the criteria for one of the specific ATPD, and four (14%) met the criteria for a non-specific ATPD. The most common diagnosis for the other cases was schizophrenia (n=16, 59%). This was largely because the duration of these cases exceeded the maximum allowable duration for ATPD (1-3 months, depending on the specific diagnosis). Again, this pattern was consistent in both developing and industrialised settings. In fact, no cases met the ATPD criteria in the industrialised settings.
Implications for ICD-10 ATPD
The introduction of ATPD in ICD-10 was an advance over other attempts at classifying remitting psychoses. The ICD-10 formulation was influenced by the classic descriptions by continental psychiatrists of such psychoses under different names such as ‘cycloid psychoses’ (Reference LeonhardLeonhard, 1961) and ‘bouffées délirantes’ (Reference PichotPichot, 1986). The growing empirical evidence for the distinctive epidemiological characteristics (Reference Susser and WanderlingSusser & Wanderling, 1994), long-term course (Reference Susser, Varma and MattooSusser et al, 1998), biological correlates (Reference Collins, Varma and WigCollins et al, 1999), and, as reported here, distinctive distribution of duration, all support the ICD-10 concept of ATPD as a nosological entity distinct from other psychotic disorders.
However, the operational criteria for ATPD in ICD-10 need refinement, so as to better capture the cases of remitting psychoses with acute onset for which they were designed. In this study, none of the cases of remitting psychoses with acute onset in the industrialised country settings, and only two cases in the developing country settings, were allocated to one of the specific ATPD categories.
We have elsewhere proposed specific revisions for ICD-10 criteria (Reference Susser, Varma and MattooSusser et al, 1998). One revision, supported by the results of the present study and our previous work (Reference Susser, Varma and MalhotraSusser et al, 1995b ), is to extend the duration criterion to 6 months. Another revision proposed is to forego the current sub-classification within the ATPD pending further research. Currently ICD-10 includes four specific and two non-specific disorders under the rubric of the ATPD (Table 1). However, as noted in the text of the ICD-10, there is little empirical evidence for such sub-classification. The small number of cases which met the criteria of ATPD in the present study did not allow us to examine the validity of this sub-classification. Indeed, as these conditions are rare in industrialised countries, where most diagnostic research is conducted, the number of patients with psychosis who would be needed to collect enough cases of each specific ATPD for validation studies would be prohibitively large. Partly for this reason, we and other authors (Reference Susser, Varma and MalhotraSusser et al, 1995b ; Reference Jørgensen, Bennedsen and ChristensenJørgensen et al, 1997) have questioned the usefulness of dividing ATPD into distinct disorders.
A fundamental difference between the ICD-10 system and the DSM-IV (American Psychiatric Association, 1994) system in regard to classification of brief psychoses is the inclusion of mode of onset as a criterion. ICD-10 ATPD are defined by acute onset, whereas DSM-IV schizophreniform disorder and brief psychotic disorder are not. A further analysis of the DOSMeD data showed that remitting psychoses with acute onset have an epidemiological distribution quite distinct from that of the remitting psychoses with non-acute onset (unpublished data available from the first author upon request). Remitting psychoses with acute onset were approximately twice as common in women and 10 times as common in the developing country settings; this was not found, however, for remitting psychoses with non-acute onset.
Implications for other ICD-10 diagnoses
Duration criteria are used to distinguish two of the ATPD diagnoses (F23.1 and F23.2; see Table 1) from schizophrenia (F20), and two other ATPD diagnoses (F23.0 and F23.3; see Table 1) from persistent delusional disorders (F22) and other non-organic psychotic disorders (F28). Revision of the ATPD duration criteria, therefore, may have repercussions on the diagnostic criteria of the other disorders. For example, if the maximum duration of ATPD is extended to 6 months, the minimum duration criterion for schizophrenia may also need to be extended to 6 months. The implications of changing the duration criteria for ATPD on the boundaries with other disorders need to be empirically assessed in future studies.
Directions for future research
As the findings from this study suggest, there is a need for additional research on remitting psychoses with acute onset. Future research will have to be on a large scale and involve a number of centres, because of the relative rarity of these disorders and because of the potential importance of the sociocultural setting. Special attention will have to be given to defining the concept of acute onset, and it seems likely that this will involve using many different sources of information, in spite of the inevitable practical difficulties.
Future research also needs to examine the symptoms of these psychoses in more depth. Classic descriptions of remitting psychoses with acute onset, such as cycloid psychoses (Reference LeonhardLeonhard, 1961) and boufées délirantes (Reference PichotPichot, 1986), gave prominence to the use of distinctive symptoms in differentiating these disorders from other psychotic disorders. Some of these features, such as polymorphic symptoms and perplexity, are mentioned in the description of ATPD in ICD-10, and if future research is successful in identifying a set of reliable and specific symptoms for these disorders, such features may be given more prominence in the future ICD editions. However, very few modern empirical studies have attempted to identify symptoms that are specific to remitting psychoses with acute onset and can distinguish these cases from cases of other psychotic disorders, and, in our own research, we have had little success in identifying such symptoms.
Limitations
The results of this study should be considered in the context of its limitations. First, the number of developing country incidence sites was limited to two, and the majority of the cases of remitting psychoses with acute onset were identified in these two sites. It is reassuring, however, that the examination of duration in the developing and in the industrialised settings in the larger sample, which included all sites, revealed remarkably similar results across the two settings as well.
Second, the criteria for ICD-10 ATPD were not developed at the time of the DOSMeD study and these disorders were not the focus of this study; therefore, no questions about the specific criteria of these disorders were included. This is particularly the case in regard to the rating of mode of onset. Acute onset in ICD-10 is operationalised as onset within 2 weeks. The closest rating to this in the DOSMeD study was the rating of onset within 1 week. The findings from the present study need to be replicated in more focused and detailed studies using specific ICD-10 criteria.
Third, ratings of mode of onset and duration of illness were often based on information obtained from a key informant who was available for the interview, and these data could not always be verified by other means (such as using multiple sources of information). However, these ratings were made using standardised instruments with established reliability within and across sites (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992).
Fourth, an ICD-9 diagnosis of schizophrenia was among the inclusion criteria for the present study. This excluded cases of ICD-9 reactive psychosis (codes 298.3, 298.4 and 298.8), even if these cases met the other criteria for remitting psychoses with acute onset. In the incidence sites of the DOSMeD, however, only one case out of the 43 with a diagnosis of reactive psychosis met the onset and duration criteria for remitting psychoses with acute onset as defined in this study. Inclusion of this case in the analyses did not change the results.
Fifth, the duration of illness before intake into the study was rated in months. This rating was less fine-grained than the rating of duration after intake, which was made in weeks. However, the median duration of illness before intake in both settings was only 1 month, and the median duration after intake was 9 weeks. More precise assessment of duration before intake, therefore, could not have changed the results of the study.
Sixth, as described earlier, for methodological reasons, cases with more than one episode during the 2-year follow-up were not included in the study. Both the classic descriptions of remitting psychoses with acute onset (Reference LeonhardLeonhard, 1961; Reference PichotPichot, 1986) and the modern clinical studies (e.g. Reference GuinnessGuinness, 1992) have noted recurrence of episodes in a subgroup of these patients. The results of the present study, therefore, need to be replicated in studies which include patients with multiple episodes.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ The modal duration of remitting psychoses with acute onset is 2-4 months.
-
▪ Mainly because of their duration, few of the cases met the criteria for ICD-10 acute and transient psychotic disorders (ATPD).
-
▪ The ICD-10 criteria for ATPD, especially in regard to duration, need to be refined so as to better capture the cases of remitting psychoses with acute onset.
LIMITATIONS
-
▪ The number of developing country sites among the incidence sites of the study was limited to two in north India.
-
▪ ‘Acute onset’ in this study was defined as onset within 1 week, whereas the ICD-10 definition of acute onset for ATPD is onset within 2 weeks.
-
▪ Ratings of mode of onset and duration of illness were often based on information obtained from a key informant and these data could not always be verified by other means.
ACKNOWLEDGEMENTS
We would like to acknowledge the contribution of the 12 World Health Organization Field Research Centers that carried out the Determinants of Outcome Study. The chief collaborating investigators were E. Strömgren, Aarhus; K. C. Dube, Agra; C. Leon, Cali; N. N. Wig and V. Varma, Chandigarh; D. Walsh, Dublin; A. Marsella and M. Katz, Honolulu; M. Olatawura, Ibadan; R. A. Nadzharov and N. N. Zharikov, Moscow; R. Takahashi and Y. Nakane, Nagasaki; J. Cooper, Nottingham; L. Hanzlicek and C. Skoda, Prague; and L. C. Wynne and T. Gift, Rochester. At the World Health Organization Headquarters, the study was coordinated by N. Sartorius, principal investigator, and A. Jablensky, co-principal investigator. R.M.'s work was supported in part by Research Career Award K01-MH01754 and Schizophrenia Research Training Grant T32-MH18870 from the National Institute of Mental Health, Rockville, MD, and by a National Alliance for Research on Schizophrenia and Depression Young Investigator Award. E.S.'s work was supported in part by Schizophrenia Research Center Grant 5P20-MH50727 and the Lieber Center. We thank Jack Gorman, MD, Evelyn Bromet, PhD, Alex Cohen, PhD, and Pamela Collins, MD for helpful comments on earlier versions of this paper.








eLetters
No eLetters have been published for this article.