Suicide is a major cause of death in mental illness, increased risk being associated with all diagnoses except dementia (Reference Harris and BarracloughHarris & Barraclough, 1997). Reducing suicide among patients with severe mental illness was a target in Health of the Nation (Department of Health, 1992). Accurate prediction of risk is difficult (Reference Allebeck, Varla and WistedtAllebeck et al, 1986; Reference ApplebyAppleby, 1992) and little is known about the protective or disruptive effect of mental health care. Although risk is highest in the month after discharge (Reference Goldacre, Seagroatt and HawtonGoldacre et al, 1993; Reference Geddes and JuszczakGeddes & Juszczak, 1995), the incidence of suicide is low. The sensitivity, specificity and positive predictive value of known risk factors is low, and therefore the number of false-positives (patients perceived as high risk who do not commit suicide) is high (Reference Goldstein, Black and NasrallahGoldstein et al, 1991). The Wessex Recent In-Patient Suicide Study (WRISS) is a retrospective case—control study designed to test the hypotheses that certain personal and clinical characteristics can predict increased risk and that continuity of care after discharge reduces risk of suicide.
METHOD
Sample size calculation
A 2:1 control—case ratio was chosen to increase the power of the study. A standard calculation at a significance level of 0.05 and a power of 80%, based on an odds ratio of 1.5, assuming a breakdown in continuity of care of 40% in living patients and 50% in deceased patients, gave a sample size of 600 living controls and 300 deceased in-patients.
Identification of recently discharged psychiatric patients
Every resident of Hampshire, Dorset, Wiltshire and the Isle of Wight (Wessex) on whom a suicide (ICD-9 E950-59) or open verdict (ICD-9 E980-89, excluding E9888) was given in the years 1988-1997 was identified from official mortality files and coroners' registers (Reference KingKing, 1983). These deaths are collectively referred to as suicides; all open verdict deaths were considered as potential suicides, because previous findings suggest that this gives a more accurate figure for overall suicides (Reference Abed and BakerAbed & Baker, 1998), and open verdicts are included within the Health of the Nation targets. Every inquest file was inspected and 373 suicides (including 92 open verdicts (25%)) were identified who died before discharge or within a year of discharge from psychiatric in-patient treatment.
Ethical approval was obtained to inspect the case notes of discharged recent psychiatric patients admitted to a hospital in the Wessex region, and matched control patients. Recent in-patients admitted to hospitals outside Wessex, to military or naval hospitals or to a special (high-security) hospital were excluded. Data were extracted from medical case notes by one psychiatrist (J.M.A.S.) and recorded on a specifically designed pro forma under the headings: Admission history; Demographic information (including legal and de facto marital status); Psychiatric history; Medical history; Index admission; Discharge data; Communication with GP; Treatment at admission and at death/follow-up; Last contact; Status of arranged psychiatric services at death/follow-up; Continuity of contact; and Changes in personnel after discharge. Two key variables were defined: whether or not there had been a break in continuity of contact and whether or not there had been a change in key personnel. Continuity of care was assessed by the number of days a patient had been ‘out of contact’, as measured by the interval between the date of a missed appointment, or self-discharge, and the date of next contact. Key personnel included keyworker, consultant or out-patient doctor.
To clarify possible ambiguities in the collection and interpretation of data, the research team compiled a manual of operationally defined criteria to which to refer. A test—retest exercise of 12 sets of notes was undertaken 12 months after the original pro forma had been completed. Kappa was calculated for every variable on the questionnaire, but only 105 variables were included in the a priori analysis. The result of the test—retest exercise showed that the kappa correlation between the two ratings was excellent (68%; κ>0.8) or very good (16%; 0.6<κ<0.8) in the vast majority of responses. None of the variables for which kappa was <0.2 (very poor) was included in the variables entered into the multiple regression model.
Matching of control patients
Each discharged index patient suicide was matched with two controls using the following sequential criteria: gender; age (age of index patient ± 10 years but not crossing adolescent/old age service boundaries); psychiatric diagnosis (schizophrenia and schizophrenia-like disorders, non-psychotic affective disorders and ‘residual’ diagnoses); ward type; and admission date. The two patients, satisfying the above criteria, whose admission dates were nearest that of the index patient (within 2 months either side) were selected. If only one suitable match could be made within this period, then a single control patient was used. If no match was admitted within 2 months, the time was extended in either direction until the closest match of the same diagnostic group was found. Patients in the ‘residual’ diagnosis group were matched as closely as possible within ICD-9 codes 300-316. Every index patient was matched with at least one control. The follow-up period for each control was the same number of days as the number of days from discharge to the event leading to death (ELD) for the index patient.
As it is well known that suicide rates vary between the different diagnoses (Reference Harris and BarracloughHarris & Barraclough, 1997; Reference Baxter and ApplebyBaxter & Appleby, 1999), patients were matched for diagnostic group to exclude this potentially confounding factor from the analysis.
Statistical procedures
Multiple conditional logistic regression (Reference CollettCollett, 1991) was carried out in STATA 6 (Stata Corp, 1999). The resulting odds ratios (ORs) for a rare event (such as suicide) give an approximate relative risk (Reference CollettCollett, 1991). A large amount of data were collected on each patient and we identified 105 potential variables to analyse. The analysis proceeded in two stages. The first was a hypothesis-testing approach in which variables that had been specified a priori were included in a model, together with potential confounders, also specified a priori. A hypothesis-generating approach was also undertaken, in which a stepwise backward elimination of variables, with probability for rejection set at 0.1, was used to produce a parsimonious model.
Clinical application
Having defined those factors that showed statistical significance between the two groups, and calculated the ORs, the sensitivity and specificity of these factors were calculated in order to assess their utility within the risk assessment process.
RESULTS
Sample
Of the 298 suicides identified, 11 non-Wessex admissions were excluded and 53 sets of case notes were untraceable (Fig. 1). Case notes of both controls were found for 84% index cases.
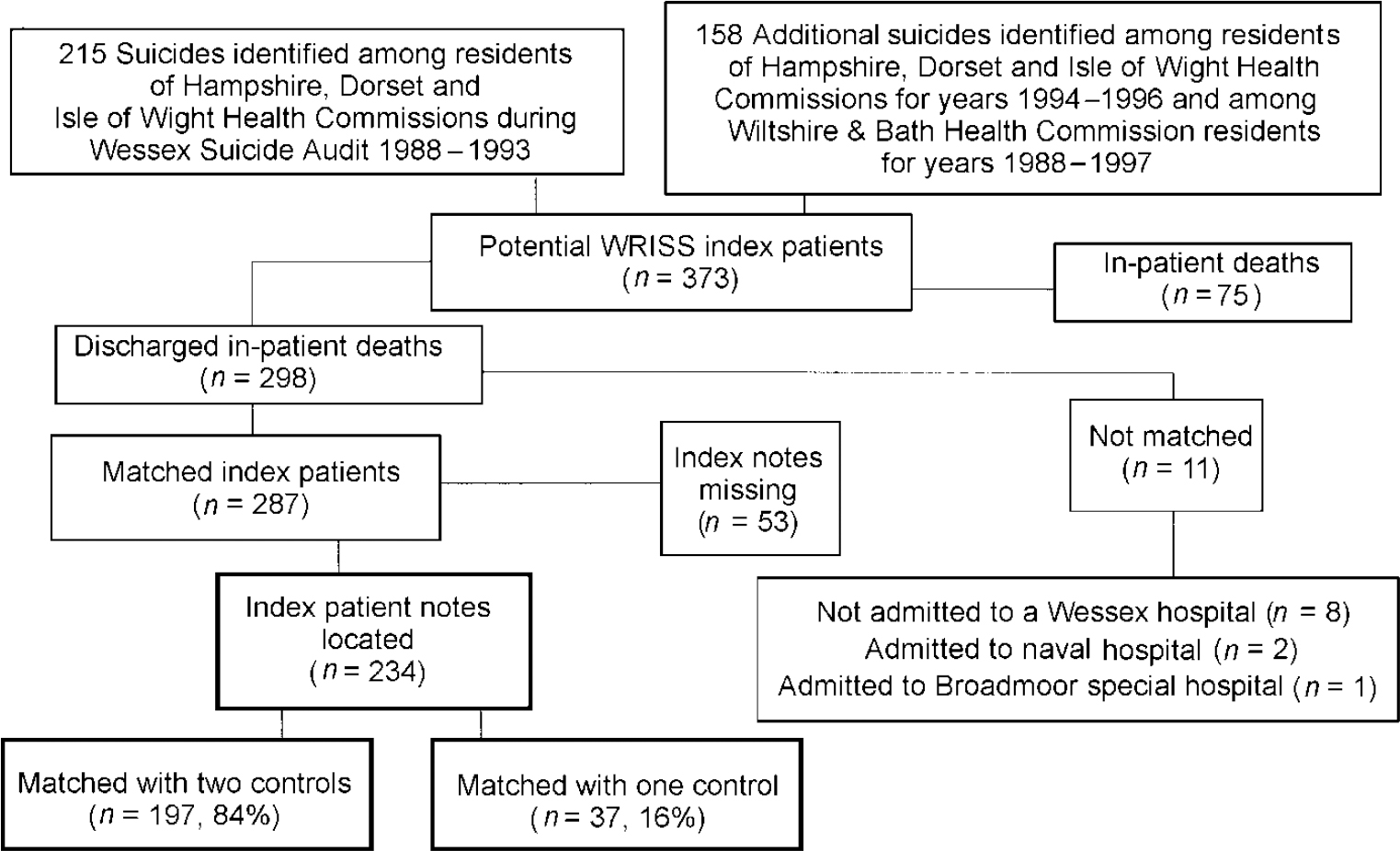
Fig. 1 Identification of 234 Wessex Recent In-Patient Suicide Study (WRISS) index recently discharged in-patient suicides.
Follow-up period
Thirty-four per cent of the 234 discharged index patients died within 28 days of discharge, 61% within 3 months and 83% within 6 months.
Clinical characteristics
Sixty-one per cent of patients were admitted to old ‘mental hospitals’, 36% to district general hospital psychiatric units and 2% to private hospitals. Eighty-nine per cent were admitted to general psychiatric open wards.
Although the index:control patients ratio was 1:1.84, the two groups were well matched for gender, age and diagnosis. The male:female ratios are 1.67:1 (index) and 1.63:1 (controls). Mean ages of male index and control patients were 42 (17-86) and 42 (18-82), and for the females 48 (15-87) and 47 (17-89) years, respectively.
The diagnostic distribution of the index patients and controls differed depending on the source of the diagnostic data (discharge register, discharge summary, Patient Administration System (PAS) computer file or case notes) but, irrespective of source, the two groups remained well-matched (Table 1).
Table 1 Diagnoses of 234 recently discharged psychiatric in-patient suicides and 431 matched controls from different sources of data
| Control group | Index group | |||
|---|---|---|---|---|
| n=431 | % | n=234 | % | |
| Diagnostic group on which matched (from discharge register or PAS file) | ||||
| Schizophrenia and schizophrenia-like disorders | 73 | 17 | 41 | 17 |
| Psychotic affective disorders | 95 | 22 | 50 | 21 |
| Non-psychotic affective disorders | 194 | 45 | 105 | 45 |
| Residual diagnoses | 69 | 16 | 38 | 16 |
| Psychiatric diagnosis at index admission (from discharge summary in case notes) | ||||
| Schizophrenia and schizophrenia-like disorders | 88 | 20 | 42 | 18 |
| Psychotic affective disorders | 78 | 18 | 39 | 17 |
| Non-psychotic affective disorders | 143 | 33 | 86 | 37 |
| Residual diagnoses | 107 | 25 | 56 | 24 |
| Others1 | 15 | 4 | 11 | 4 |
| Primary psychiatric diagnosis (from case notes) | ||||
| Schizophrenia and schizophrenia-like disorders | 93 | 22 | 43 | 18 |
| Bipolar affective disorder | 58 | 13 | 22 | 9 |
| Non-psychotic depressive illness | 198 | 46 | 123 | 53 |
| Anxiety/phobia/panic disorder/obsessive—compulsive disorder | 6 | 1 | 3 | 1 |
| Eating disorder | 2 | 1 | 3 | 1 |
| Alcohol misuse and/or dependence | 43 | 10 | 19 | 8 |
| Substance misuse and/or dependence | 4 | 1 | 4 | 2 |
| Personality disorder | 13 | 3 | 9 | 4 |
| Dementia | 3 | 1 | 0 | 0 |
| Others1 | 11 | 2 | 8 | 3 |
Results of conditional logistic regression analysis
Table 2 shows the results of fitting a logistic regression model in which the three variables associated with a breakdown in continuity of care were included, along with potential confounders. This result was consistent for a variety of different confounders: history of deliberate self-harm (DSH); admission because of suicidal ideas; evidence of delusions/hallucinations, depressive symptoms, feelings of hopelessness and evidence of misuse of non-prescribed substances (excluding alcohol) at admission; and DSH during admission.
Table 2 Independent factors associated with breakdown in care: results of multiple regression model1
| Controls | Index | Odds ratio | P | |
|---|---|---|---|---|
| (n=431) | (n=234) | (95% Cl) | ||
| Key personnel on leave/leaving | 4 (0.9%) | 12 (5.1%) | 18.45 (4.46-76.32) | <0.001 |
| Continuous contact between discharge and ELD/follow-up | 275 (63.8%) | 120 (51.3%) | 0.57 (0.37-0.87) | 0.010 |
| Change of consultant since previous admission | 231 (53.6%) | 147 (62.8%) | 1.63 (1.09-2.44) | 0.016 |
Continuity of contact
Although about 70% of both groups were in contact with the psychiatric service at the time of ELD/follow-up, significantly more control patients had remained in continuous care (no periods of time ‘out of contact’) compared with index patients. Continuous care was associated with a decreased risk of suicide.
Continuity of professional carers
A key professional being on leave, or leaving, at the time of the fatal act was associated with a near 17-fold increase in suicide risk, but this occurred in only 5% of the suicides.
Factors associated with changed risk of suicide
Table 3 shows the final model, which explores the data set to find significant predictors of suicide.
Table 3 Independent variables remaining after backward elimination from multiple conditional logistic regression model
| Variable | Control group | Index group | Odds ratio (95% Cl) | P | ||
|---|---|---|---|---|---|---|
| n=431 | % | n=234 | % | |||
| Factors associated with increased suicide risk | ||||||
| Key personnel on leave or leaving | 4 | 1.0 | 12 | 5.3 | 16.82 (3.54-79.80) | <0.001 |
| Becoming unemployed | 5 | 1.2 | 12 | 6.3 | 7.88 (2.09-29.71) | 0.002 |
| New relationship problems | 7 | 1.7 | 11 | 4.9 | 4.89 (1.13-21.15) | 0.033 |
| History of DSH | 179 | 44.3 | 157 | 69.8 | 4.09 (2.58-6.48) | <0.001 |
| Not planned discharge | 151 | 35.0 | 125 | 53.4 | 2.73 (1.77-4.22) | <0.001 |
| DSH during admission | 14 | 3.2 | 19 | 8.1 | 2.57 (1.00-6.62) | 0.050 |
| Not White | 23 | 5.3 | 24 | 10.2 | 2.22 (1.04-4.75) | 0.039 |
| Suicidal ideas at index admission | 170 | 39.4 | 130 | 55.8 | 1.93 (1.22-3.06) | 0.005 |
| Living alone | 135 | 31.3 | 95 | 40.6 | 1.87 (1.19-2.93) | 0.006 |
| Evidence of hopelessness | 58 | 14.4 | 62 | 27.6 | 1.82 (1.04-3.19) | 0.035 |
| Admitted under new consultant1 | 231 | 53.6 | 147 | 62.8 | 1.56 (1.01-2.41) | 0.042 |
| Factors associated with reduced suicide risk | ||||||
| Received continuous care | 275 | 68.1 | 120 | 53.3 | 0.63 (0.40-1.00) | 0.050 |
| Evidence of delusions at index admission | 125 | 30.9 | 44 | 19.6 | 0.48 (0.26-0.86) | 0.014 |
| Misuse of non-prescribed substances | 44 | 10.9 | 16 | 7.1 | 0.39 (0.17-0.88) | 0.023 |
| Admitted from shared accommodation | 32 | 7.9 | 8 | 3.6 | 0.28 (0.10-0.77) | 0.014 |
Social factors
The only social factor associated with increased suicide risk was living alone, whereas admission from shared accommodation was associated with a reduced risk. Shared accommodation included supported group homes and sharing with friends: those living in unsupported hostels were considered to be living alone.
Clinical factors
The two groups were similar in respect of Mental Health Act status at index admission but differed in the reason for admission and information elicited on history and mental state examination. A history of DSH, admission because of suicidal ideation and mental state examination findings of hopelessness all increased the risk of suicide. Neither a family history of suicide nor a family history of mental illness changed the risk. Patients admitted with psychotic features (delusions or hallucinations) or misuse of non-prescribed substances occurred more frequently in the control group, despite being matched for diagnosis, than in those who ultimately committed suicide following their subsequent discharge.
Events during admission
Only the onset of new relationship difficulties was significantly associated with an increased risk of suicide.
Events after discharge
Personal events
Loss of job between admission and ELD/follow-up was associated with a sevenfold increase in suicide risk.
Cumulative effects
Of those who went on to commit suicide: 32% had at least four increased suicide risk factors present, compared with only 9% of the control group; and only 3.4% of the index cases had none of the identified risk factors, compared with 15.5% of the control group. However, none of the index cases individually had more than seven of the eleven factors present.
Sensitivity and specificity
As this is a case—control study, the positive predictive value (PPV) of the risk factors cannot be ascertained because the prevalence is fixed at 33% (two controls per case), and the PPV depends on the prevalence of a condition within the sample population.
DISCUSSION
This case—control study has identified eleven factors associated with increased risk of suicide, and four factors associated with decreased risk, in the year following discharge from psychiatric in-patient care.
Table 4 Independent variables associated with reduced suicide risk: sensitivity and specificity

| Variable | Sensitivity | Specificity |
|---|---|---|
| Key personnel on leave or leaving | 0.05 | 0.99 |
| Becoming unemployed | 0.05 | 0.99 |
| New relationship problems | 0.05 | 0.98 |
| History of DSH | 0.67 | 0.58 |
| Not planned discharge | 0.53 | 0.65 |
| DSH during admission | 0.08 | 0.97 |
| Not White | 0.10 | 0.96 |
| Suicidal ideas at index admission | 0.56 | 0.61 |
| Living alone | 0.41 | 0.69 |
| Evidence of hopelessness | 0.26 | 0.87 |
| Admitted under different consultant | 0.63 | 0.46 |
| Presence of > 3 factors | 0.32 | 0.91 |
Limitations
The study has three limitations. The first is that it relies on data collected retrospectively from medical case notes that were not intended to be used for research purposes. The fact that no information was recorded in clinical notes in relation to a particular aspect of care does not mean that the information was not known at the time. However, because decision-making in health care is based on existing information, comprehensive and accurate recording is a prerequisite for effective communication between professionals. Data not available for this study were presumed not to be available to the professionals treating the patient. As Bachrach (Reference Bachrach1981) has argued, communication or continuity of information, implies the existence of relevant and adequate case records that are readily available to all involved providers of health and social care.
The second limitation is that it was impossible to blind the research fellow responsible for completing the data pro forma to the patient outcome. To minimise possible bias, questions were made objective and were based only on explicit information recorded in the case notes.
The third limitation is that many variables (105) were analysed but these were identified as potential variables a priori. With any modelling procedure some allowance should be made for multiple tests. Five of the positive risk factors have a P value of ≤0.005 and so would remain significant if a Bonferroni correction were applied.
Strengths
This study has the strength of being a large case—control study, with a comprehensive sample drawn from a population of 2.9 million (1991 Census, all ages; Office of Population Censuses and Surveys, 1991). All patients received in-patient treatment from at least one mental health facility within a single regional health authority administrative area. Although the study was not prospective in design, at the time of index admission and discharge all staff were in effect ‘blind’ as to which one of the three in-patients would die within the following year.
Previous findings
A retrospective case—control study of 63 discharged in-patient suicides (Reference Dennehy, Appleby and ThomasDennehy et al, 1996) reported that ‘conventional’ risk factors, such as unemployment and living alone, were as common among cases as controls. These factors are characteristic of people with severe mental illness in general and do not predict risk in individual psychiatric patients. A subsequent report (Reference Appleby, Dennehy and ThomasAppleby et al, 1999) on 149 patients also reported no significantly increased suicide risk associated with these variables.
New findings
In this larger study with two controls per index patient we found that nine of the eleven increased-risk factors are associated with personal or clinical characteristics, supporting our first hypothesis.
Readmission under the same consultant and continuous contact with the same professionals are associated with decreased risk. This provides support for the second hypothesis and emphasises the importance of continuity of both contact and personnel, especially in vulnerable groups. However, this statistically significant result may be an artefact of the retrospective nature of the study, with bias in the recording of events with hindsight, and would need to be evaluated in prospective studies.
Several potential factors may explain why patients admitted with psychotic features (delusions/hallucinations) were significantly less likely to commit suicide ultimately. The first is that patients with these symptoms may be considered in need of hospital admission for treatment, without additionally needing to be considered ‘at risk’ of suicide to justify their hospital admission. Alternatively, the answer may lie in ‘treatability’ of severe mental illness and the consequent reduction that this has on mortality.
It is often considered difficult to maintain contact with some patient groups, particularly those with alcohol/drug dependence or a comorbid Axis II disorder. However, in this study the ORs for continuity of care were not altered significantly when analysed using these as a confounding factor. The OR changed from 5.7 to 5.2 (95% CI 0.36-0.75). One of the key statements of the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness is: “Suicides with alcohol or drug dependence or personality disorder had the most disrupted pattern of care, including high rates of loss of contact with services” (Department of Health, 1999). Our findings suggest that, when compared with controls with the same diagnosis, this effect is less specific to the suicide group and more of a reflection of general factors within this population.
The finding that misuse of nonprescribed substances appeared to be a protective factor against suicide requires further exploration. Previous studies have found high rates of suicide in those who misuse alcohol or drugs (Reference Appleby, Shaw and AmosAppleby et al, 1997; Reference Harris and BarracloughHarris & Barraclough, 1997). This group is more likely to receive a verdict of accidental death rather than suicide (Reference KingKing, 1990). Accidental death verdicts were not included in this study and so rates were expected to be lower. Alternatively, suicide rates in those who were not correctly identified as having substance misuse might be particularly high, and the identification and management of these conditions may be protective. A recent study of in-patient suicides (Reference Powell, Geddes and DeeksPowell et al, 2000) found that substance misuse was associated with a reduced risk of suicide and postulated that patients admitted for these problems were not as acutely ill as some other patients and do not have the same suicide risk.
At index admission, the only significant social differences between the index and control patients were in de facto marital status and living alone. The only independent pre-admission clinical factor associated with an increased risk of suicide was a history of DSH. This is consistent with the findings of a similar case—control study (149 cases) (Reference Appleby, Dennehy and ThomasAppleby et al, 1999).
Representativeness of sample
A comparison between the social, demographic and clinical characteristics of the WRISS patients who died within 3 months of discharge and the corresponding 519 suicides reported to the National Confidential Inquiry (Department of Health, 1999) suggests that the Wessex suicides are a representative group. The lower prevalence of schizophrenia among WRISS patients may be because there are relatively fewer urban conurbations in Wessex than in the rest of England and Wales.
Implications for clinical practice
The highest risk of suicide in discharged in-patients occurs immediately after leaving hospital, suggesting that flexible community support should be made available at an early stage. However, the incidence of suicide in this group is low: between 1 in 500 and 1 in 1000 of the patients discharged (Reference GeddesGeddes, 1999).
The 16-fold increase in risk when a significant professional was on leave, or about to go on leave, at the time of the fatal act indicates that a break in the continuity of the carer may be a final precipitating factor in predisposed individuals. This is consistent with the ‘relationship’ element in continuity of care as described by Bachrach (Reference Bachrach1981): “the patient's ability to rely, over time, on having an association with a person or persons who are interested in him/her and who respond to him/her on a personal level”.
Information about the increased suicide risk associated with post-discharge social events could be useful to general practitioners, who may feel that they have little responsibility for the mental health of their patients if they are currently under the care of psychiatric services. However, they are often contacted and are frequently the last contact that the patient has with a health professional prior to suicide (Reference KingKing, 2001).
Awareness of the identified risk factors for suicide after discharge could be used to structure risk assessments at discharge and at subsequent reviews. The numerical values associated with these risk factors could allow serial assessment of a current ‘risk score’ by health-care professionals both when caring for psychiatric in-patients and when engaged in their long-term follow-up. This score could become part of regular multi-disciplinary discussions, with documentation of the score within the Care Programme Approach process. Mental health services then could be delivered in a flexible fashion, with increased intervention at times of higher risk and lesser involvement during periods of low risk. However, there will be a significant false-positive rate, which will have resource and ethical consequences if treatment and discharge decisions are based solely upon a ‘risk score’.
The low sensitivity and specificity of identified risk factors confirm the findings of previous studies (Reference Appleby, Dennehy and ThomasAppleby et al, 1999; Department of Health, 1999). Identifying which patients are at higher risk of suicide remains an inexact science.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ In discharged patients, one-third of suicides occurred within the first month after discharge.
-
▪ It is possible to identify factors associated with the outcome of suicide in recently discharged patients, but the utility of these factors remains uncertain.
-
▪ Continuity of contact may reduce suicide risk.
LIMITATIONS
-
▪ Data were collected retrospectively from medical case notes that were not originally intended for research purposes, and data collection was not carried out blind to case—control status.
-
▪ The sensitivity and specificity of the identified risk factors are low.
ACKNOWLEDGEMENTS
Thanks are due to: Professor Andrew Stevens (Department of Public Health, University of Birmingham), who helped to develop the protocol; Dr Sarah Goode, who matched all the index patients with two controls and located the notes; Lorna Campbell, for administrative support and data entry; and all the coroners, clinicians and medical records staff, without whose cooperation this study would not have been possible. The Research Support Subcommittee of the University of Southampton provided some additional funding.










eLetters
No eLetters have been published for this article.