Formal thought disorder has long been regarded as one of the cardinal symptoms of schizophrenia. Although thought disorder is most apparent during acute episodes of illness, the chronic phase of schizophrenia is characterised by vague, wandering speech (Reference Spohn, Coyne and LarsonSpohn et al, 1986). Continuation of thought disorder after the resolution of an acute psychotic episode is a strong predictor of poor outcome (Reference Norman, Malla and CorteseNorman et al, 1999). However, formal thought disorders, especially the less florid forms characteristic of the chronic phase of the illness, are difficult to assess. One difficulty in the evaluation of formal thought disorder arises from the clinical observation that the manifestation of thought disorder depends on the form and content of the clinical interview. Substantial evidence indicates that formal thought disorder reflects abnormalities in the executive control of language (Reference McGrathMcGrath, 1991). Executive control entails planning, organising and monitoring. The degree to which executive control is required depends on the extent to which the speaker is responsible for determining the content of the spoken output. A standardised assessment of thought disorder should evaluate verbal output produced under standardised circumstances in which the patient none the less has substantial autonomy in determining the content of the output.
In recent decades one of the most widely used instruments for assessing formal thought disorder has been the Thought, Language and Communication (TLC) scale, devised by Andreasen (Reference Andreasen1979). Subsets of TLC items are incorporated in the positive thought disorder sub-scale of the Scale for the Assessment of Positive Symptoms (SAPS) and in the alogia sub-scale of the Scale for the Assessment of Negative Symptoms (SANS) (Reference AndreasenAndreasen, 1987). The TLC scale provides concise definitions of many aspects of thought disorder. However, in a comprehensive review, Straube & Oades (Reference Straube and Oades1992) concluded that the TLC scale is not sensitive to subtle anomalies such as those that occur in relatives of patients. In contrast, the Thought Disorder Index (TDI) devised by Johnston & Holzman (Reference Johnston and Holzman1979) was designed to measure a wide range of disorders, including quite subtle anomalies. The TDI entails assessment of speech during two standardised procedures: responding to Rorschach ink-blots, and completing the Wechsler Adult Intelligence Scale. The use of a procedure that is standardised, yet gives the patient substantial executive responsibility for speech generation, is likely to provide sensitivity and reliability without sacrificing validity. However, the TDI is too time-consuming for routine clinical use, and the scoring of disorders requires extensive training (Reference Johnston and HolzmanJohnston & Holzman, 1979).
Wynne & Singer (Reference Wynne and Singer1963) employed Rorschach ink-blots to elicit communication deviance in the families of patients with schizophrenia. They described a variety of aspects of communication deviance, including responses that are confused, vague, incomplete, or involve odd usage of words, that could be detected in the parents of patients with schizophrenia. Employing these researchers' concept of communication deviance in a prospective longitudinal study, Goldstein (Reference Goldstein1985) observed communication disturbances in families that were detectable before the onset of schizophrenia in the identified patient.
METHOD
The Thought and Language Index
The Thought and Language Index (TLI) is a new instrument for assessing formal thought disorder under standardised conditions. It is based on principles embodied in Wynne & Singer's concept of communication deviance and in Johnston & Holzman's TDI, but is much briefer. The patient is required to produce eight 1-min speech samples in response to standard stimuli from either the Thematic Apperception Test (Reference MurrayMurray, 1943) or the Rorschach test (Reference RorschachRorschach, 1942). The speech samples are assessed for the presence of eight types of abnormality, which are defined in a glossary and scored according to specified criteria (see Appendix). Two items (poverty of speech and weakening of goal) reflect impoverishment of thought and speech. Four items (looseness, peculiar word use, peculiar sentence construction and peculiar logic) are phenomena reflecting the disorganisation of thought and language that is characteristic of psychotic disorders, especially schizophrenia. We shall refer to these four items as disorganisation phenomena. In addition, the TLI includes two nonspecific abnormalities of the regulation of speech and thought (perseveration and distractibility). These are not specific to psychotic illnesses, but none the less are relatively common in psychotic illnesses.
The study reported here was designed to test the reliability and factor structure of the TLI items, and the prevalence of these abnormalities in patients with schizophrenia and in healthy control individuals. Whether or not the overt disorganisation of thought that occurs in schizophrenia is on a continuum that embraces the mild oddities of speech and thought discernible in healthy individuals has been a subject of debate. This is a part of the larger debate regarding the prevalence of psychotic symptoms, perhaps attenuated in severity, in a healthy population (Reference Van Os, Hanssen and Bijlvan Os et al, 2000). In the TLI, individual instances of disordered thought or language are assigned a score of 0.25, 0.50, 0.75 or 1.0, depending on severity. A score of 0.25 indicates that the abnormality of the phenomenon is questionable. For example, in scoring ‘peculiar word use’, the use of a rare word when a more common word would convey the meaning more clearly would be rated 0.25. A score of 0.25 for ‘looseness’ would be assigned for ‘intrusion of loosely related or unrelated ideas, after which the subject immediately returns to the original train of thought’. If the disorganisation of thought characteristic of schizophrenia lies on a continuum that embraces the mild aberrations of speech and thought discernible in healthy individuals, it would be predicted that disorganisation item scores of 0.25 would be observed in healthy participants and in those with schizophrenia. Furthermore, a positive correlation between the prevalence of items scored at 0.25 and the prevalence of items scored at 0.50 or above would be expected.
Participants
Two samples of patients satisfying ICD—10 criteria for schizophrenia (World Health Organization, 1992) were recruited: 49 patients from Ealing Hospital, London, UK, and 38 patients from Vancouver Hospital, Canada. The Ealing patients were predominantly people with severe, chronic illness undergoing rehabilitation, either in hospital or in the community. Their mean age was 43.6 years and 41 were male. The participants from Vancouver were mainly in the resolving phase of an acute psychotic episode. They were assessed a mean of 24 days after admission to an acute psychiatric ward. Their mean age was 35.0 years and 21 were male. All patients in both samples were receiving treatment with antipsychotic medication. In addition, 24 healthy participants with a mean age of 32.4 years, 13 of whom were male, were recruited by advertisement in Vancouver and matched in age and gender to 24 of the Vancouver patients. The healthy participants had no current psychiatric illness, no personal history of psychotic illness and no history of psychotic illness in a first-degree relative. The procedure was approved by the ethics review committees of Ealing Health Authority and the University of British Columbia.
Assessment procedure
The TLI was administered to each participant and scored according to the TLI manual (details available from the author upon request). Eight pictures from the Thematic Apperception Test were presented sequentially for 1 min each, and the participant was asked to talk about each picture. If the person stopped speaking before the minute was over, a non-directive prompt (e.g. ‘Can you say more?’) was given. At the end of the minute, the interviewer asked the person tested to explain any odd or unusual utterances that had been made during the minute. After this enquiry phase, the next picture was presented. The entire procedure lasted approximately 15 min. The interview was recorded on audiotape and subsequently transcribed. The SANS and the SAPS were administered to the Vancouver group.
Interrater reliability
For the purpose of assessing interrater reliability of the TLI, the transcripts of 25 interviews from the Vancouver study group were scored independently by five assessors (four psychology graduate students and a psychiatrist) who had participated in six training sessions each of approximately 1-h duration, conducted by the author of the scale (P.F.L.). Interrater reliability was quantified using intraclass correlation coefficients (ICCs) (Reference Bartko and CarpenterBartko & Carpenter, 1976).
Factor analysis
Scores for TLI items for the entire sample of 87 participants were subjected to factor analysis using the Statistical Package for the Social Sciences (SPSS, 1999). Initial factors were extracted using the method of principal factors, and subjected to oblique rotation using the oblimin procedure.
Comparison with healthy controls
For the purpose of comparing TLI item prevalence in patients with that in healthy participants, the transcripts of the interviews with the 24 healthy people and 24 matched patients from the Vancouver sample were scored by an assessor who was blind to diagnostic status. The severity of TLI item scores in each group were compared using the Mann—Whitney test. To test the hypothesis that thought disorders typical of schizophrenia occur in attenuated form in healthy individuals, the prevalence of item scores at level 0.25 for the four disorganisation phenomena was compared in healthy participants, in patients without definite disorganisation (i.e. without any disorganisation phenomena scored at level 0.5 or above) and in patients with definite disorganisation phenomena. The significance of differences in prevalence between the three groups was assessed according to the Kruskal—Wallis test, using SPSS for Windows Release 10.0.05 (SPSS, 1999). In addition, the Spearman correlation between prevalence of disorganisation phenomena scored at level 0.25 and the prevalence of disorganisation phenomena scored at level 0.5 or greater was computed.
Relationship of TLI sub-scales to SANS and SAPS sub-scales
The Spearman correlation between the TLI disorganised thought/language sub-scale score (sum of scores for looseness, peculiar word use, peculiar sentence construction, peculiar logic) and the SAPS positive thought disorder global score was computed for the Vancouver sample. Similarly, the correlation between TLI impoverished thought/language sub-scale score (sum of scores for poverty of speech and weakening of goal) and the SANS alogia global score was computed.
RESULTS
Interrater reliability
The ICCs assessing interrater reliability of individual TLI items ranged for 0.60 for peculiar word use to 0.93 for poverty of speech (Table 1). The ICC for the impoverished thought/language sub-scale was 0.88, and that for the disorganised thought/language sub-scale was 0.82.
Table 1 Interrater reliability for Thought and Language Index items and sub-scale scores
| Item | ICC |
|---|---|
| Impoverished thought/language | |
| Poverty of speech | 0.93 |
| Weakening of goal | 0.74 |
| Disorganised thought/language | |
| Looseness | 0.79 |
| Peculiar word | 0.60 |
| Peculiar sentence | 0.75 |
| Peculiar logic | 0.77 |
| Non-specific dysregulation | |
| Perseveration | 0.77 |
| Distractibility | 0.70 |
| Sub-scale scores | |
| Impoverished thought/language | 0.88 |
| Disorganised thought/language | 0.82 |
Factor analysis
The factor analysis revealed three factors with eigenvalues greater than 1.0, which together accounted for 71% of the shared variance. The factor loadings, after oblique rotation, are shown in Table 2. The four disorganisation items loaded heavily on the first factor; the two impoverishment items loaded heavily on the second factor; and perseveration and distractibility loaded on the third factor. The first factor reflected the existence of significant mutual correlations, ranging from 0.29 to 0.60, between the four disorganisation items. The second factor reflected a strong correlation of 0.76 (P≤0.001) between poverty of speech and weakening of goal. The third factor reflected the existence of a moderate correlation between perseveration and distractibility (r=0.41, P<0.001). All pair-wise correlations between factors were trivially small (less than 0.15 in absolute magnitude).
Table 2 Oblique factor analysis of Thought and Language Index items
| Item | Factor loadings | ||
|---|---|---|---|
| Poverty of speech | -0.16 | 0.92 | -0.06 |
| Weakening of goal | -0.08 | 0.89 | 0.10 |
| Looseness | 0.66 | 0.03 | 0.38 |
| Peculiar word | 0.78 | -0.17 | -0.13 |
| Peculiar sentence | 0.72 | -0.37 | -0.03 |
| Peculiar logic | 0.74 | 0.04 | 0.10 |
| Distractibility | 0.21 | 0.35 | 0.76 |
| Perservation | -0.08 | -0.19 | 0.87 |
Comparison of patients with controls
The mean severity of TLI items (and the sub-scale scores) in the Ealing patient sample, and in the 24 matched patients and controls from Vancouver, are shown in Fig. 1. Although the mean severity of TLI items was substantially less in healthy control individuals than in the matched Vancouver patients, the scores in the healthy control group were not negligible. However, apart from one instance of looseness and one peculiar sentence (each scored at level 0.5) in one healthy individual, and one peculiar sentence scored at level 0.5 in another, the scores in healthy participants were accumulated from items scored at level 0.25, which denotes phenomena of questionable abnormality.
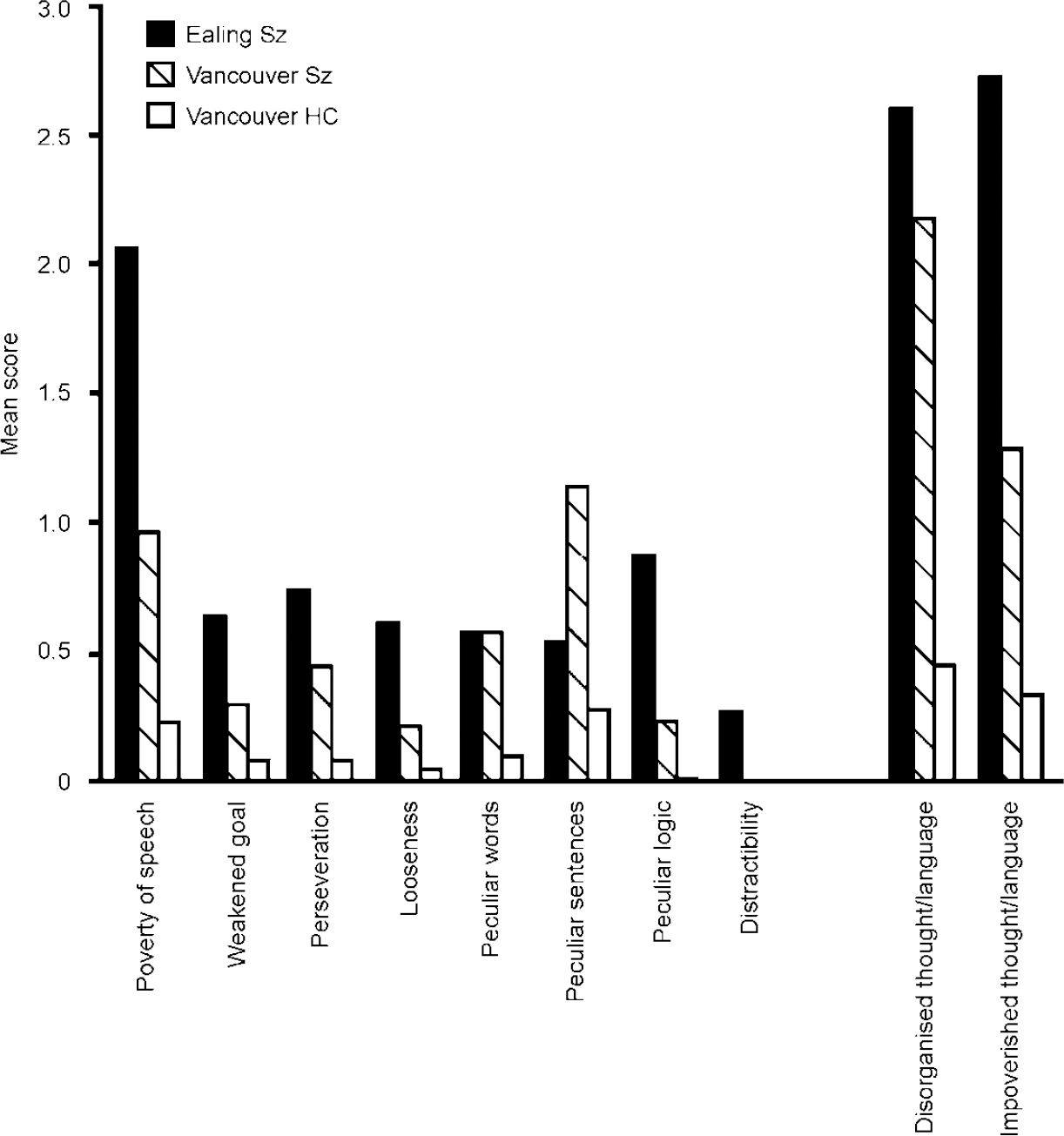
Fig. 1 Mean severity of Thought and Language Index items and sub-scale scores (disorganised thought/language; impoverished thought/language) in the Ealing schizophrenia (Sz) group (n=49), the Vancouver schizophrenia matched sample (n=24) and the matched healthy controls (HC; n=24). The difference between the Vancouver schizophrenia sample and the matched healthy control groups was significant at the level P≤0.05 (Mann—Whitney test) for both sub-scale scores and for all individual items (except distractibility, which was rated zero in these patients and controls).
The mean number of disorganisation phenomena scored at level 0.25 was 1.8 per person for healthy control participants. From the matched sample of 24 patients, 12 had no definite evidence of disorganised thought/language (i.e. no individual disorganisation phenomenon scored at the level 0.5 or above). For these 12 patients the number of disorganisation phenomena scored at level 0.25 was 3.6 per person, whereas for the 12 patients with definite evidence of disorganised thoght/language the number was 9.0 per person. The difference between these three groups in the prevalence of phenomena scored at level 0.25 was significant (Kruskal—Wallis test, χ2=16.0, d.f.=2, P<0.001). Comparison of pairs of groups demonstrated that patients with definite disorganisation exhibited significantly more phenomena scored at level 0.25 than both the healthy control group (Mann—Whitney U=26.5, P<0.001) and the patients without definite disorganisation (U=27, P=0.009). However, the patients without definite evidence of disorganisation did not differ significantly from the healthy control individuals in the number of phenomena scored at level 0.25 (U=118.8, P=0.38). The Spearman correlation between the prevalence of disorganisation phenomena scored at level 0.25 and the prevalence of disorganisation phenomena scored at level 0.5 or above was 0.615 (P<0.001).
Correlations with SANS and SAPS scores
The correlation between the TLI disorganisation sub-scale score and the SAPS positive thought disorder global score was 0.49 (P=0.001), and the correlation between the TLI poverty of thought sub-scale and the SANS alogia global score was 0.40 (P=0.001).
DISCUSSION
Psychometric properties of the TLI
The interrater reliability for TLI items ranged from satisfactory to excellent, and the reliability for the disorganisation and impoverishment sub-scales was excellent. The factor structure revealed by factor analysis indicates that disorders of the flow and form of thought in schizophrenia segregate into three almost orthogonal groups. These groups comprise items reflecting impoverished thought and language; disorganised thought and language of the type commonly regarded as characteristic of psychotic illnesses; and non-specific dysregulation of thought. The near-orthogonality of these groups of phenomena suggests that the underlying pathophysiological processes are almost independent. It should be noted that to minimise risk of bias, during the training of the raters who scored the speech transcripts in this study the distinction between items reflecting impoverishment, disorganisation and non-specific dysregulation was not discussed, although the distinction between negative phenomena (reflecting diminished amount of mental activity) and positive phenomena (reflecting the presence of abnormal mental activity) was discussed.
Item severity scores
In the Ealing patient group, predominantly people with severe chronic illness, poverty of speech was the item with greatest mean severity. It is noteworthy that all aspects of disorganised thought/language were relatively common, despite the fact that the amount of speech produced by these patients was low. In the Vancouver patient group, who were predominantly in the resolving phase of an acute psychotic episode, peculiar sentence construction had the highest mean severity. Poverty of speech was appreciable, but less severe than in the more chronic sample from Ealing.
The severity of TLI item scores in the healthy participants was much lower than in the matched Vancouver patients, but not negligible. The order of items when ranked according to mean severity was similar in the healthy control group to that in the Vancouver patients. Distractibility was rare or absent in all groups assessed in this study. However, this item has been retained in the TLI because distractible speech is relatively common in patients acutely ill with psychosis, especially in those with mania.
The continuum of severity of disorganisation
The finding that mild aberrations of thought and language occur in healthy individuals but are more prevalent in people with schizophrenia and, furthermore, that the prevalence of these mild aberrations is correlated with the prevalence of more severe, clearly abnormal disorders, suggests that there might be a continuum of severity of disorganised thought in the human population. The occurrence of such a continuum would have important implications for the nature of psychotic thought disorder, suggesting that this disorder might arise from one or more causal factors that exert an influence widely in the population. However, it should be noted that on account of the small sample size in this study, further investigation is warranted to confirm the existence of a continuum of severity of formal thought disorder in the population at large.
Relationship to SANS and SAPS sub-scales
The significant correlation between TLI sub-scale scores and SANS and SAPS thought disorder sub-scale scores confirms that the phenomena elicited by the TLI overlap with the phenomena scored using SANS and SAPS. However, the modest magnitude of the correlations demonstrates that the phenomena revealed by the TLI are not identical to those assessed by SANS and SAPS. The question of which scales provide the most valid measurement of thought disorder in schizophrenia is unlikely to be answered until the intrinsic nature and pathological mechanism of formal thought disorder have been established.
TLI scores and the pathophysiology of thought disorder
An additional feature of the TLI is its suitability for use in functional imaging studies where it is necessary to elicit the phenomena of interest within a standard frame-work and within a time frame of several minutes. It has been used successfully in a positron emission tomography study by McGuire et al (Reference McGuire, Quested and Spence1998) and a functional magnetic resonance imaging study by Kircher et al (Reference Kircher, Liddle and Brammer2001). Both of these studies found that severity of positive thought disorder is correlated with decreased activation of language areas in the left superior temporal gyrus, and with abnormal function of the anterior cingulate cortex, a brain region engaged in the executive control of behaviour and speech. The consistency of these findings suggests that the TLI is a valid measure of language disorder in schizophrenia. This conclusion receives further support from the finding by Kuperberg et al (Reference Kuperberg, McGuire and David1998) that positive thought disorder assessed by the TLI was associated with reduced sensitivity to linguistic violations during a word monitoring task.
The TLI is a reliable measure of thought and language disorders that is sensitive to subtle disorders which are prevalent in schizophrenia and discernible in healthy individuals. The existing evidence indicates that it quantifies phenomena related to specific deficits in linguistic performance and to specific patterns of aberrant brain activity. Studies of the relationships between TLI scores, abnormalities of cognition assessed by the techniques of cognitive psychology and regional cerebral activity assessed by neuroimaging, offer the prospect of further delineation of the mechanism of formal thought disorder in both psychological and neurological terms.
CLINICAL IMPLICATIONS
-
▪ The Thought and Language Index (TLI), which employs standard stimuli to elicit eight brief speech samples, provides sensitive and reliable measurements of thought and language disorders in schizophrenia.
-
▪ Disorganisation and impoverishment of thought and language in schizophrenia are approximately orthogonal rather than bipolar: that is, they can coexist, but are almost independent phenomena. Non-specific dysregulation of speech (perseveration and distractibility) is independent of both impoverishment and disorganisation.
-
▪ Comparison of TLI scores in patients and healthy control participants suggests that there is a continuum of severity of disorganised thought and language in the human population.
LIMITATIONS
-
▪ The size of the healthy control group was too small to justify detailed analysis of the prevalence of individual TLI items in these participants.
-
▪ Unmedicated patients with acute schizophrenia were not studied.
-
▪ The exclusion of patients with affective psychosis prevents conclusions about the specificity to schizophrenia of TLI phenomena scored at level 0.5 or above.
APPENDIX
Definitions of Thought and Language Index items
Guidelines for assigning scores can be obtained from the author of the scale (P.F.L.).
- Poverty of speech
-
Poverty of speech refers to a decrease in the amount of speech. Responses to the picture and replies to questions are brief and lack elaboration.
- Weakening of goal
-
Weakening of goal reflects a lack of drive in thinking and is manifest in lack of normal elaboration of ideas, use of uninformative generalisations and empty speech that conveys little information. Weakening of goal might be accompanied by poverty of speech (diminished amount of speech), but not necessarily so. The essential issue is lack of information in proportion to the number of words spoken.
- Perseveration of ideas
-
Unwarranted repetition of ideas or themes. Increased weighting is given to instances in which the repetition occurs independently of the stimulus provided by the picture.
- Looseness
-
The connection between ideas is tenuous or absent, or extraneous ideas intrude into the train of thought. Looseness can be manifest during a spontaneous train of thought — designated ‘derailment’ by Andreasen (Reference Andreasen1979) — or by virtue of irrelevant or tangential replies to questions — designated ‘tangentiality’ by Andreasen.
- Peculiar use of words
-
Unusual or invented words are used. If the word is used more than once in the response to a single picture, rate only the first use, but consider the possibility of scoring perseveration of ideas when the inappropriate word is used repeatedly.
- Peculiar sentences
-
The form of the sentences is unusual. Greater weight is given to peculiarity of sentence construction, which makes it difficult to discern the meaning. Sentences with grammatical inaccuracies attributable to poor education should not be rated as peculiar.
- Non-logical reasoning (peculiar logic)
-
Conclusions are reached based on inadequate evidence or faulty logic. The judgement that an utterance reflects peculiar logic should be made after the enquiry phase. It is essential that the examiner should note all unusual ideas expressed during the free response phase, and make a subsequent enquiry into the basis for these ideas. Allow any reasonable speculation. If an inappropriate utterance is based only on perseveration, it is not rated as peculiar logic. However, if the person gives an irrational explanation for an instance of perseveration, occurrences of both perseveration and peculiar logic should be recorded.
- Distractibility
-
Intrusion of extraneous ideas arising from an external stimulus.








eLetters
No eLetters have been published for this article.