The Human Rights Act 1998 and the Race Relations (Amendment) Act 2000 place responsibilities on service providers to eradicate discriminatory procedures and practice. Inequitable variation in use of health care services between ethnic groups concerns policy makers, patients and clinicians (Reference AchesonAcheson, 1998; Department of Health, 2000). A previous review reported that mental health services are unattractive to some ethnic groups, who complain of more coercive treatments and adverse experiences (Reference Cochrane and SashidharanCochrane & Sashidharan, 1996). Although this perception has become widespread, studies that compare access and use of mental health services by different ethnic groups have not been reviewed systematically. It is not known how consistently the findings suggest poorer access for minority ethnic groups, or how these findings relate to study design and methodological quality (Reference Cochrane and SashidharanCochrane & Sashidharan, 1996). We undertook a review of the published studies on ethnic variations in use of primary care or mental health services in the UK.
METHOD
Our review focused on specific questions: is there variation between ethnic groups in (a) pathways to specialist mental health care; (b) continuing contact with mental health services; (c) use of in-patient services; and (d) compulsory admissions. We included published papers that compared access to, or use of, primary or secondary mental health care in the UK by at least two ethnic groups with psychotic and non-psychotic mental disorders in primary and secondary care (see Appendix). We excluded specialist services for children, adolescents and older people, as well as forensic services and services for psychosexual disorders or substance misuse.
The following bibliographic databases were searched: ASSIA, CINAHL, the Cochrane Trials Register, EMBASE, HealthStar, Medline, PsycLIT, Science Citation Index and SIGLE. The search was restricted to studies published in English between January 1983 and October 2000 inclusive. We identified titles and abstracts of papers that potentially fulfilled our inclusion criteria. The grouped search terms included: (a) GREAT BRITAIN, HEALTH SERVICES, INDIGENOUS ETHNIC GROUP; (b) HOSPITALS, PSYCHIATRIC, MENTAL HEALTH SERVICES, PSYCHIATRY, MENTAL DISORDERS, PSYCHOTROPIC DRUGS; (c) ETHNIC or MULTI-ETHNIC, UK or BRITAIN or LONDON, MENTAL or PSYCHIATRY or PSYCHOTROPIC. In databases where MESH terms were available they were exploded and combined. Searches were adapted for the different databases and performed independently by two reviewers. These searches were supplemented by personal bibliographies of the investigators, forward citation tracking using the Science Citation Index and Social Science Citation Index databases and by references in retrieved articles. We sent a list of all included studies to three external experts, asking them to identify any other relevant studies.
Abstracts, if available, or full papers were assessed independently by two reviewers. All potentially relevant papers were then assessed against inclusion and exclusion criteria. Disagreement was resolved by a third reviewer. Data were extracted independently by two reviewers. Discrepancies were resolved by discussion or by a third reviewer. For studies reporting pathways to specialist mental health care, continuing contact with mental health services and use of in-patient services, we conducted a narrative review because differences in the measurement and reporting of outcomes made combination of point estimates inappropriate. The narrative analysis involved comparison of tabulated data and appraisal of methodological quality (see below). For the review of variation in compulsory admissions to in-patient facilities, in addition to a narrative review, we performed a meta-analysis to quantify variation between ethnic groups in compulsory admission to in-patient facilities. We have expressed the main results as combined odds ratios with the random effects method after performing tests for heterogeneity. We combined data on the proportions of White and Black patients who were compulsorily admitted in the primary studies. We examined publication bias and related biases in a funnel plot and carried out a test of funnel plot asymmetry. All analyses were performed with StatsDirect (http://www.statsdirect.com/).
Two reviewers independently assessed the methodological quality of each published study, with criteria adapted from Raine's review of gender differences in health service use (Table 1; Reference RaineRaine, 2000). We assessed the quality of published studies in four domains: sample source and size; method of ethnic group classification; adjustment for disease and confounding variables, including socio-economic status; and whether ethnic groups were combined appropriately in the analysis. Each of these was equally important in the allocation of quality score. Papers varied in their classification of ethnic groups and these were often aggregated into broad categories. In our analysis we have used the most commonly reported aggregated categories, comparing ‘Black’ and ‘South Asian’ groups with ‘White’ participants. We summarised the results of the papers and examined whether quality scores, geographical location of the research, the composition of the ethnic groups and study design could explain any heterogeneity of findings.
Table 1 Scoring system for methodological quality of paper
| Sample source and size | Score | Adjustment for confounding variables | Score | Ethnicity categorisation | |||
|---|---|---|---|---|---|---|---|
| Quality | Score | Use in the analysis | Score | ||||
| Routine data (e.g. health authority, GP list data) | 0 | None | 0 | Third-party reports (e.g. ward staff categorisation, name-based methods, skin colour methods) | 0 | Inappropriate ethnic groups combined for major study outcomes (e.g. Blacks v. all others) or poor method of collecting ethnicity data | 0 |
| Project-specific data: <30 cases in ethnic groups for major outcomes | 1 | Age and/or gender | 1 | Self-reported ethnicity or use of census categories | 1 | Lumping of groups: reasonable combinations of groups collected by census/self-report method | 1 |
| Project-specific data: >30 cases in ethnic groups for major outcomes | 2 | Diagnosis or disease severity (give 1 point if this sample is selected by diagnosis) | 1 | All analysis done on ethnic groups without amalgamation, and self-report/census categories for categorisation | 2 | ||
| Project-specific data: total sample size >500 | 3 | Comorbidity and risk factors for outcome of interest1 | 1-3 | ||||
| Maximum possible2 | 3 | 5 | 1 | 2 | |||
RESULTS
Primary studies identified and quality scores
A total of 545 potentially relevant titles and abstracts were identified. Sixty-seven papers were scrutinised. One duplicate publication was excluded, leaving 38 papers that met our criteria (see Appendix). One additional paper that was identified by an external reviewer did not meet our inclusion criteria. Details of each paper, including classification of ethnic groups, demographic characteristics, study design and quality ratings are summarised in Table 2 (the full review tables can be seen on the Institute of Community Health Sciences Queen Mary website at http://www.ichs.qmul.ac.uk/transcultural/TMS-Pub1.htm). Quality scores ranged from 0 to 11 and were summarised into three categories: low quality (0-3); medium quality (4-7); and high quality (8-11). There were five high-quality and 23 medium-quality studies. The total quality score was most highly correlated with adjustment for confounders (r=0.81) and methods for ethnic group classification (r=0.6). The more recently published papers achieved higher quality scores (r=0.57, P=0.0002).
Table 2 Characteristics of studies included in review (ethnic classifications and diagnoses are those used in the original studies)

| Author (ethnic definition1) | Ethnic groups reported, n (%) | Actual sample size, n (% response rate) | Diagnoses, n (%)2 | Sample source | Data source | Design and follow-up | Other variables in analysis | Quality |
|---|---|---|---|---|---|---|---|---|
| Reference Bebbington, Feeney and FlanniganBebbington et al, 1994 (D) | Black Caribbean 71 | 376 | Psychosis 195 | IP | Probably MR | CS, 1-day census and admission over subsequent 91 days | Age, gender, informal or formal admission, challenging behaviour, emergency or not sections | 6 |
| White 305 | Affective disorder 140 | |||||||
| Other 41 | ||||||||
| Reference Bhugra, Corridan and RudgeBhugra et al, 1999 (D) | Asian 24 | 62 (100) | Schizophrenia | IP, OP, GP | MR, Int | 5 | ||
| White 38 | ||||||||
| Reference Bindman, Johnson and SzmuklerBindman et al, 2000 (B) | White 49 | 97 (74) | SMI (all together) | Community sample of prevalent cases | MR, Int | CS, collected prospectively | Living alone, admission to hospital | 6 |
| Black Caribbean 34 | ||||||||
| Black African 11 | ||||||||
| Asian 3 | ||||||||
| Reference Birchwood, Cochrane and MacmillanBirchwood et al, 1992 (D) | Indian 30 | 101 (73) | Schizophrenia 62 | CMHT, IP | MR; contact with CMHT | CP, 12-month historical cohort | Age, gender, SES | 3 |
| African—Caribbean 50 | Psychosis NOS 30 | |||||||
| White English 74 | ||||||||
| Irish 5 | ||||||||
| Other 10 | ||||||||
| Reference Burnett, Mallett and BhugraBurnett et al, 1999 (C) | African—Caribbean 38 | 100 | Schizophrenia 100 | IP, OP, GP, Pris, CMHT | MR, Quest, Int | 2-year prospective data collection but a CS pathways study | Age, gender, SES | 7 |
| White 38 | ||||||||
| Asian 24 | ||||||||
| African—Caribbean 183 | Schizophrenia 809 | 20-year historical cohort using Camberwell Register | ||||||
| White 626 | ||||||||
| Reference CallanCallan, 1996 (A) | African—Caribbean, M: 24, F: 26 | 134 (100) | Schizophrenia | IP | MR | Prospective CP, matched case—control | Age, gender, SES | 7 |
| White British, M: 24, F: 17 | ||||||||
| Reference Castle, Phelan and WesselyCastle et al, 1994 (A+D) | White 79 | 484 (90) | Schizophrenia | IP, OP, CMHT | MR, Case register | FCPsych 19-year historical cohort | Age, gender, SES | 4 |
| African—Caribbean 78 | Paraphrenia | |||||||
| Other | ONPsych | |||||||
| UK, Eire, West Indies, Africa, Asia, Other | ||||||||
| Reference Cole, Leavey and KingCole et al, 1995 (B) | White 39 | 93 (88) | Schizophrenia 58 | IP | Quest, Int | Retrospective CS | Age, gender, unemployment | 8 |
| Black 38 | Other 35 | |||||||
| Asian 16 & other | ||||||||
| Reference Commander, Dharan and OdellCommander et al, 1997b (B) | Asian 1516 | GenPop 433 (28.9) | Schizophrenia 38.5/48.73 | IP, OP, CMHT, GP. | MR, Quest, Int | CS, 6-months prospective admissions | Age, gender, SES | 5 |
| Black 3068 | GP 834 (74) | BAD 7.7/12.73 | GenPop, For, Pris | |||||
| White 1195 | OP psychiatric services 2451 | Depression 12.3/11.83 | ||||||
| Neurosis 18.4/6.93 | ||||||||
| IP specialist (including | Drug misuse 4.5/6.33 | |||||||
| For) 834 | None 11.8/4.93 | |||||||
| Other 6.8/8.73 | ||||||||
| Reference Commander, Dharan and OdellCommander et al, 1997c (B) | As above | As above | As above | As above | As above | As above | Age, gender | 5 |
| Reference Commander, Cochrane and SashidharanCommander et al, 1999 (B) | Asian 40 | 120 (100) | NAPsych (all) | IP | Int | Retrospective, CP at admission (120) and discharge (120) | 5 | |
| Black 40 | ||||||||
| White 40 | ||||||||
| Reference Crowley and SimmonsCrowley & Simmons, 1992 (D) | African—Caribbean/ | 152 (100%) | Psychosis 86 | IP | MR | CS, Age- and gender-matched case—control | Age, gender, SES | 2 |
| Asian 77 | Organic 7 | |||||||
| White 75 | Mania 10 | |||||||
| Neurosis 39 | ||||||||
| Personality disorder 7 | ||||||||
| Reference Davies, Thornicroft and LeeseDavies et al, 1996 (A+B) | Black African 29 | 213 (93) | Schizophrenia 238 | IP, OP, GP, CMHT | MR | CS, all prevalent cases of psychosis in a sector, retrospective | Age, number of admissions living alone | 9 |
| Black Caribbean 115 | APsych 13 | |||||||
| Black other 15 | Other psychosis 188 | |||||||
| White 254 | Total psychosis 439 | |||||||
| Reference Dunn and FahyDunn & Fahy, 1990 (D) | White 165 | 268 (100) | Schizophrenia 88 | IP | MR, Quest | CP | Age, gender | 3 |
| Black 88 | Hypomania 52 | |||||||
| Asian 7 | Depression 11 | |||||||
| Uncertain 8 | Drug-induced psychosis 24 | |||||||
| Personality disorder 22 | ||||||||
| Reference Falkowski, Watts and FalkowskiFalkowski et al, 1990 (D) | African—Caribbean | 100 | Schizophrenia 45 | IP who asbscond | MR, CS | CS, retrospective | 2 | |
| 26 | BAD 17 | |||||||
| African 8 | PPsych 9 | |||||||
| UK/Irish 49 | Personality disorder 8 | |||||||
| Other European 10 | Neurosis 21 | |||||||
| Asian 6 | ||||||||
| Other 1 | ||||||||
| Reference Flannigan, Glover and FeeneyFlannigan et al, 1994 (D) | White (66.4/76.8)4 | CS 147 | Psychosis | IP | MR | CP | Age, gender, SES | 3 |
| Black Caribbean (22.9/15.8)4 | Prospective 266 | |||||||
| Other (10.8/7.4)4 | ||||||||
| Reference GloverGlover et al, 1989 (A) | Jamaica | 2466 (73.9) | All psychiatric, schizophrenia, mania, depression | IP | RD | Historical cohort using Mental Health Enquiry data over 3 years (1982-1985) | Gender | 4 |
| Barbados | ||||||||
| Trinidad/Tobago | ||||||||
| Reference Goater, King and ColeGoater et al, 1999 (B+C) | White 39 | 93 (73 at year 1, 71 at year 5) | Schizophrenia 35 | IP, OP, CMHT, GP, AE, For, Pris | MR | Prospective incidence cases | Age, gender, SES | 7 |
| Black 38 | NAPsych 22 | Quest | ||||||
| Asian 11 | APsych 22 | Int | ||||||
| Other 5 | ||||||||
| Reference GuptaGupta, 1991 (A) | Asian 86 | 172 | Psychosis | IP, CP | MR | FCPsych, 5-year cohort | Age, gender | 6 |
| White 86 | ||||||||
| Reference Harrison, Holton and NeilsonHarrison et al, 1989 (D) | African-Caribbean 42 | 131 (100) | Psychosis 42 | IP, OP, CMHT | MR, Quest, Int | CS, FCPsych | Age, gender | 4 |
| RSch 28 | ||||||||
| General population 89 | ||||||||
| Reference Ineichen, Harrison and MorganIneichen et al, 1984 (D) | White—UK 193 | 264 (100) | All diagnoses where there was compulsory admission | IP | MR | Retrospective, CS | Gender | 4 |
| West Indian 43 | ||||||||
| Other non-White 19 | ||||||||
| Other White 9 | ||||||||
| Reference Koffman, Fulop and PashleyKoffman et al, 1997 (B) | White (75) | 3710 (93.2) | Schizophrenia | IP | MR, survey | CS, I-day census | Age, gender | 5 |
| Black (15) | ||||||||
| Asian (4) | ||||||||
| Reference Lloyd and MoodleyLloyd & Moodley, 1992 (D) | Black 37 | 128 (95.2) | Schizophrenia 59 | IP | MR, Int | One-day census of IP | Age, gender, compulsory detention | 5 |
| Non-Black 101 | BAD 31 | |||||||
| Other psychosis 11 | ||||||||
| Neurosis 9 | ||||||||
| Other non-Psych 15 | ||||||||
| Unknown 9 | ||||||||
| Reference McCreadie, Leese and Tilak-SinghMcCreadie et al, 1997 (D) | Black Caribbean 131 | 468 | Schizophrenia 468 | IP, OP, GP, CMHT | MR, Quest | CS | Age, gender | 4 |
| White 337 | ||||||||
| Reference McGovern and CopeMcGovern & Cope, 1987 (A+B) | White 511 | 587 (100) | Schizophrenia/PPsych 71 | IP | MR | CS | Age, gender | 5 |
| African—Caribbean 72 | ||||||||
| British-born African—Caribbean 41 | Affective disorder 56 | |||||||
| Cannabis psychosis 17 | ||||||||
| Other 102 | ||||||||
| Reference McGovern and CopeMcGovern & Cope 1991 (A+C) | African—Caribbean 33 | 62 (87) | Schizophrenia | IP | MR | CS | 4 | |
| White 29 | ||||||||
| Reference McKenzie, van Os and FahyMcKenzie et al, 1995 (A+C) | African—Caribbean 53 | 113 | Psychosis | IP | MR, Int | Cohort | 10 | |
| White 60 | Mean follow-up at 49 months (African—Caribbean) at 44 months (White) | |||||||
| Total 191 | ||||||||
| Reference Moodley and ThornicroftMoodley & Thornicroft, 1988 (A) | West Indian 26 | 100 (100) | Schizophrenia 75 | IP | MR, Quest combined | CS, CP | Age, gender, SES | 2 |
| Other 9 | Affective 165, Other psychosis 55 | |||||||
| White 65 | ||||||||
| Reference Moodley and PerkinsMoodley & Perkins, 1991 (D) | African—Caribbean (48) | 52 (86.7) | Schizophrenia (40.4) | IP | MR, Int | CP, CS | Age, gender, SES | 3 |
| White (42) | BAD (25.5) | |||||||
| Depression (27.7) | ||||||||
| Reference Odell, Surtees and WainwrightOdell et al, 1997 (B) | White | 752 (72) | GHQ score | Practice lists | Int, MR | CS | GHQ score, gender of GP, psychiatric history, physical health | 10 |
| African—Caribbean | 125 GPs in 66 practices | |||||||
| Asian | ||||||||
| Reference Owens, Harrison and BootOwens et al, 1991 (C) | African—Caribbean 120 | 275 (100) | Schizophrenia and PSchizo 114 | IP | MR, Int | Prospective | Age, gender, marital, PA, PCA | 4 |
| White UK-born 120 | ||||||||
| Depression 63 | ||||||||
| Mania 41 | ||||||||
| Other psychosis 23 | ||||||||
| Neurosis, personality disorder, none 30 | ||||||||
| Reference Parkman, Davies and LeeseParkman et al, 1997 (A+B) | White (UK-born) 114 | 184 (63) | Schizophrenia 59 | CP in contact with SS, GPs, sheltered accommodation, voluntary, private, and self-help care; clergy; homeless and prison services | MR, Quest, Int | CS, of random sample of prevalent cases of psychoses in contact with specified agencies | Age, gender, SES | 9 |
| White (non-UK-born) 20 | APsych 7 | |||||||
| Other NAPsych 30 | ||||||||
| Black Caribbean (UK-born) 27 | ||||||||
| Black Caribbean (non-UK-born) 23 | ||||||||
| Reference Perkins and MoodleyPerkins & Moodley, 1993 (D) | White (48) | 52 (86) | Schizophrenia (40.4) | IP, CP | MR, Int | CS | Age, gender, PA, MHA, GPI, PI | 3 |
| African—Caribbean (42) | BAD (25.5) | |||||||
| Reference Singh, Croudace and BeckSingh et al, 1998 (B+C) | Black Caribbean 44 | 417 (86.7) | Psychosis 233 non-Psych 3 | IP | Quest | CP, prospective | Age, gender, SES, psychosis, risk of violence | 9 |
| Asian 21 | ||||||||
| White 352 | ||||||||
| Reference Takei, Persaud and WoodruffTakei et al, 1998 (A+D) | White 54 | 88 (81) | Schizophrenia, Non-schizo | IP admissions in 1973/4 followed up 18 years later | MR, Quest, Int | Prospective follow-up | Age, gender, SES, age at first onset | 6 |
| African—Caribbean 34 | ||||||||
| Reference Thomas, Stone and OsbornThomas et al, 1993 (A+C) | UK-born 1363 | 1692 | All | IP | MR | CP, retrospective, CS | Age, gender, SES | 5 |
| European | Schizophrenia | |||||||
| African—Caribbean6 126 | BAD | |||||||
| African—Caribbean7 67 | ||||||||
| Asian (Indian/Pakistani)6 62 | ||||||||
| Asian7 74 | ||||||||
| Reference Turner, Ness and ImisonTurner et al, 1992 (C) | African—Caribbean 50 | 100 (63) | Schizophrenia 75 | IP | MR | Retrospective, prospective | Age, gender, SES | 4 |
| African 13 | Mania 25 | |||||||
| Caribbean 36 | Personality disorder | |||||||
| Asian 1 | 22 | |||||||
| European other 50 | Psychosis 14 | |||||||
| UK White 38 | Organic 16 | |||||||
| European 6 | Depression 2 | |||||||
| Cypriot 1 | Other 7 | |||||||
| Irish 5 | None 8 | |||||||
| Unknown 12 | Unknown 13 | |||||||
| Reference van Os, Castle and Takeivan Os et al, 1996 (B) | White 44 | 110 | NAPsych 110 | IP | MR | CS, retrospective | Age, gender | 5 |
| African—Caribbean 29 | (including 79 cases of RDC-based schizophrenia) | |||||||
| African 32 | ||||||||
| Other 5 |
Methodological findings
Most papers reported observational studies in health service settings using a cross-sectional design, without making a distinction between incident and prevalent cases (see Table 2). A total of 34 studies included information from medical records, 15 from direct interview and 10 used questionnaires. Clearly the majority of studies are therefore subject to recall bias and information bias, and where samples were recruited from in-patient and out-patient services, selection bias is likely to be important. Only three studies were of a prospective cohort design in which biased assessment of risk factors is minimised. As far as could be judged, potential biases due to study design did not explain heterogeneity. Thirty-five papers included Black participants; eight did not distinguish between people of African—Caribbean and African origin. Eight papers included South Asians as a separate category but did not distinguish between people of Pakistani, Indian or Bangladeshi origin. Six papers identified White subgroups but none analysed them separately. Ten papers used country of birth alongside ethnicity information. Nineteen studies did not use ethnic group census categories; studies collecting data before 1991 used proxy measures for ethnic group, such as place of birth. Thirteen papers did not give any explanation for their classification of ethnic groups. Most papers included small numbers of participants from each ethnic group. Twenty-eight papers adjusted for age, 28 for gender and 16 for some measure of socio-economic status, with 24 taking measures to address potential confounding due to variation in diagnoses or illness severity. Although socio-economic status is known to be a confounder in studies of ethnic variations in health, papers adjusting for it did not always score highly on the total quality scores. None of the papers reported sample size calculations. The majority of studies (26) investigated services in London; other locations were Birmingham (McGovern & Cope, Reference McGovern and Cope1987, Reference McGovern and Cope1991; Reference Birchwood, Cochrane and MacmillanBirchwood et al, 1992; Commander et al, Reference Commander, Odell and Sashidharan1997a ,Reference Commander, Dharan and Odell b , Reference Commander, Cochrane and Sashidharan1999), Manchester (Reference Thomas, Stone and OsbornThomas et al, 1993), Nottingham (Reference Harrison, Holton and NeilsonHarrison et al, 1989; Reference Owens, Harrison and BootOwens et al, 1991; Reference Singh, Croudace and BeckSingh et al, 1998) and Bristol (Reference Ineichen, Harrison and MorganIneichen et al, 1984).
Do pathways to specialist care vary with ethnic group?
Black patients had more-complex pathways to specialist services, seeing at least three carers before contact with specialist services (Reference Commander, Cochrane and SashidharanCommander et al, 1999). Compared with White patients, a greater proportion of Black patients had some contact with a helping agency the week before psychiatric service contact (Reference Harrison, Holton and NeilsonHarrison et al, 1989) and admission was more likely to follow a domiciliary visit (Reference Commander, Odell and SashidharanCommander et al, 1997a ). Compared with White and South Asian patients who visited their general practitioner (GP), Black people were less likely to be referred to specialist services (Reference Thomas, Stone and OsbornThomas et al, 1993; Reference Cole, Leavey and KingCole et al, 1995; Reference Burnett, Mallett and BhugraBurnett et al, 1999). An explanation might be the GPs' lower likelihood of recognising a psychiatric problem in Black people (Reference Odell, Surtees and WainwrightOdell et al, 1997; Reference Bhugra, Corridan and RudgeBhugra et al, 1999; Reference Burnett, Mallett and BhugraBurnett et al, 1999). However, among patients presenting to general practice who are recognised to have a mental health problem, Black patients were more likely to be found in specialist services (Commander et al, Reference Commander, Dharan and Odell1997b ,Reference Commander, Dharan and Odell c ). The police were more likely to be involved in admissions or readmissions of Black people (Reference Thomas, Stone and OsbornThomas et al, 1993; Reference Burnett, Mallett and BhugraBurnett et al, 1999; Reference Commander, Cochrane and SashidharanCommander et al, 1999). These three papers had medium-quality scores, as did one showing that police involvement before admission was explained by a lack of GP involvement rather than ethnic origin of the patients (Reference Cole, Leavey and KingCole et al, 1995). Two medium-quality papers found that Black people were most likely to present in crisis, often seeing the duty psychiatrist in an accident and emergency department as a first point of contact with services (Reference Turner, Ness and ImisonTurner et al, 1992; Reference Cole, Leavey and KingCole et al, 1995). In contrast, a low-quality paper showed no variation between ethnic groups in the pathways to specialist care (Reference Moodley and PerkinsMoodley & Perkins, 1991). Variation in the diagnostic categories and differences in ethnic group composition do not explain the heterogeneous outcomes of these studies.
In west London, specialist referral following primary care assessments appeared to be equally common among White and South Asian patients, but hospital admission was more likely among South Asians following a domiciliary visit (Reference Bhugra, Corridan and RudgeBhugra et al, 1999; Reference Burnett, Mallett and BhugraBurnett et al, 1999). In Birmingham, South Asians had the highest community rates of mental disorder, were the most frequent consulters in primary care and were less likely than White people to have their mental disorder recognised (Commander et al, Reference Commander, Dharan and Odell1997b ,Reference Commander, Dharan and Odell c ). Of all ethnic groups with a mental disorder, South Asians were the least likely to be referred to specialist care (Reference Commander, Dharan and OdellCommander et al, 1997b ; Reference Odell, Surtees and WainwrightOdell et al, 1997). Quality ratings were similar for papers from Birmingham and London and do not explain the different findings. However, the two papers reporting no variation in detection between South Asians and Whites contained smaller samples (total South Asians=24) than studies detecting significant differences (total South Asians=1516).
Is contact between specialist services and Black and South Asian people maintained?
Compared with White patients, services were less likely to maintain contact with non-Whites in one part of south London (Norwood) but not in another neighbouring area (Nunhead; Reference McCreadie, Leese and Tilak-SinghMcCreadie et al, 1997). Another paper from London found no variation between ethnic groups in continuity of community care (Reference Bindman, Johnson and SzmuklerBindman et al, 2000), whereas African—Caribbean people in Birmingham had more ‘broken contact’ with aftercare services (Reference McGovern and CopeMcGovern & Cope, 1991). All three of these papers were of medium quality with a cross-sectional design and specifically recruited African—Caribbean people. The study with the largest sample size found differences between geographical areas, suggesting that variation in local service configuration and practice are influential and that ethnicity alone does not account for variations in patient contact (Reference McCreadie, Leese and Tilak-SinghMcCreadie et al, 1997).
In two papers from London, compared with White people, Black people were more likely to be in contact with services at 5- and 18-year follow-up, respectively (Reference Takei, Persaud and WoodruffTakei et al, 1998; Reference Goater, King and ColeGoater et al, 1999). These papers were of medium quality and both recruited Black people of Caribbean origin. There were no papers that looked specifically at the pattern of South Asian peoples' contact with specialist services.
Use of in-patient services
Of 20 papers on in-patients, 17 reported measures of in-patient service use (representation on in-patient units (13) consistently showed greater use of in-patient services by Black people (Reference McGovern and CopeMcGovern & Cope, 1987; Reference Owens, Harrison and BootOwens et al, 1991; Reference Birchwood, Cochrane and MacmillanBirchwood et al, 1992; Reference Thomas, Stone and OsbornThomas et al, 1993; Reference Flannigan, Glover and FeeneyFlannigan et al, 1994; Reference CallanCallan, 1996; Reference van Os, Castle and Takeivan Os et al, 1996; Commander et al, Reference Commander, Dharan and Odell1997b ,Reference Commander, Dharan and Odell c ; Reference Koffman, Fulop and PashleyKoffman et al, 1997; Reference McCreadie, Leese and Tilak-SinghMcCreadie et al, 1997; Reference Parkman, Davies and LeeseParkman et al, 1997; Reference Takei, Persaud and WoodruffTakei et al, 1998). One of these positive studies was of high quality and nine were of medium quality. Two papers (of low quality) found no variation in in-patient service use (Reference Ineichen, Harrison and MorganIneichen et al, 1984; Reference Castle, Phelan and WesselyCastle et al, 1994). One paper, a first-incidence study, found an excess of in-patient use by White patients (Reference Goater, King and ColeGoater et al, 1999). A study of admissions found an excess of admissions among Black women in one London borough but a 40% lower admission rate compared with White women in another borough (Reference Bebbington, Feeney and FlanniganBebbington et al, 1994). Quality scores and differences in the ethnic composition of the samples, as far as this could be judged, do not account for this heterogeneity. The evidence most consistently suggests an excess use of in-patient facilities by Black patients. Two papers on first-contact (incident) admissions indicate no excess among Black people (Reference Castle, Phelan and WesselyCastle et al, 1994; Reference Goater, King and ColeGoater et al, 1999), despite adjustment for age, gender and socio-economic status in one paper (Reference Goater, King and ColeGoater et al, 1999). Among patients of Caribbean origin, Jamaicans had the highest annual admission rates to British hospitals (Reference GloverGlover, 1989).
Despite variation in study quality, geographical region and South Asian group composition and different degrees of adjustment for confounders and diagnosis, results for in-patient use were more consistent for South Asians than for Black patients. Compared with Black patients, South Asians were less likely to be admitted for in-patient care, had the lowest admission rates to secure wards (Reference Commander, Dharan and OdellCommander et al, 1997c ; Reference Koffman, Fulop and PashleyKoffman et al, 1997), had shorter admissions than other ethnic groups (Reference GuptaGupta, 1991) and were least likely to be readmitted (Reference Birchwood, Cochrane and MacmillanBirchwood et al, 1992). Compared with White patients, South Asians were more likely to be admitted to in-patient care (Reference Commander, Dharan and OdellCommander et al, 1997b ; Reference Koffman, Fulop and PashleyKoffman et al, 1997).
Compulsory admissions
Of 23 papers measuring compulsory admissions, the majority (18) showed a higher rate for Black compared with White patients (Reference Ineichen, Harrison and MorganIneichen et al, 1984; Reference Moodley and ThornicroftMoodley & Thornicroft, 1988; Reference Harrison, Holton and NeilsonHarrison et al, 1989; Reference Dunn and FahyDunn & Fahy, 1990; Reference Moodley and PerkinsMoodley & Perkins, 1991; Reference Owens, Harrison and BootOwens et al, 1991; Reference Birchwood, Cochrane and MacmillanBirchwood et al, 1992; Reference Crowley and SimmonsCrowley & Simmons, 1992; Reference Lloyd and MoodleyLloyd & Moodley, 1992; Reference Perkins and MoodleyPerkins & Moodley, 1993; Reference Thomas, Stone and OsbornThomas et al, 1993; Reference Davies, Thornicroft and LeeseDavies et al, 1996; Reference Koffman, Fulop and PashleyKoffman et al, 1997; Reference McCreadie, Leese and Tilak-SinghMcCreadie et al, 1997; Reference Parkman, Davies and LeeseParkman et al, 1997; Reference Singh, Croudace and BeckSingh et al, 1998; Reference Takei, Persaud and WoodruffTakei et al, 1998; Reference Commander, Cochrane and SashidharanCommander et al, 1999). Eight of these adjusted for age, gender and socio-economic status. Two adjusted for other potential confounders: class; past admissions; Mental Health Act status (compulsory admission for assessment or detention); police involvement; and general population representation (Reference Perkins and MoodleyPerkins & Moodley, 1993; Reference McKenzie, van Os and FahyMcKenzie et al, 1995). Other papers adjusted for age at first contact (Reference Takei, Persaud and WoodruffTakei et al, 1998), psychosis, risk of violence and diagnosis (Reference Singh, Croudace and BeckSingh et al, 1998). One paper that adjusted for first-contact admissions, past admissions and marital status showed excess admissions among Black people (Reference Owens, Harrison and BootOwens et al, 1991), challenging reports that the absence of a relative or intimate relationship accounts for compulsory admission (Reference Cole, Leavey and KingCole et al, 1995). Davies et al (Reference Davies, Thornicroft and Leese1996) recruited people with psychosis from a broad range of services. After adjustment for living alone as well as for age and total number of previous admissions, this paper still found excess compulsory admissions among Black people. Although papers reporting on in-patients suggest that a higher rate of readmissions and absconding explained the excess of compulsory admissions among Black people (Reference Falkowski, Watts and FalkowskiFalkowski et al, 1990; Reference Thomas, Stone and OsbornThomas et al, 1993), Davies et al (Reference Davies, Thornicroft and Leese1996) adjusted for previous admissions and still found higher rates of compulsory admissions among Black people.
Some papers reported contradictory findings. For example, a medium-quality paper showed that, compared with White women, Black women were less likely to be voluntarily admitted in one London borough (South Southwark), but were more likely to be voluntarily admitted in another London borough (Hammersmith & Fulham; Reference Bebbington, Feeney and FlanniganBebbington et al, 1994). Such differences probably reflect variations in local practice and services. The majority of papers, using a variety of ethnic group measures and study designs and adjusting for a number of potential confounders, provide strong evidence for a relative excess of compulsory admissions of Black people.
Of three papers investigating compulsory admissions among South Asian patients, two low-quality papers found that these were less common among South Asian patients (Reference Birchwood, Cochrane and MacmillanBirchwood et al, 1992; Reference Crowley and SimmonsCrowley & Simmons, 1992). One medium-quality paper found no difference between South Asian and White patients (Reference Thomas, Stone and OsbornThomas et al, 1993). These findings are inconclusive as all three studies relied on routinely collected data from medical records and included small numbers of South Asian people.
We calculated a summary odds ratio from the 12 papers (Fig. 1) that reported the exact proportions of compulsorily admitted Black and White in-patients and sample sizes. The meta-analysis gave a pooled odds ratio (Blacks compared with Whites) of 4.31 (95% CI 3.33-5.58). Analysis of the funnel plot did not show evidence of publication bias (P=0.69).
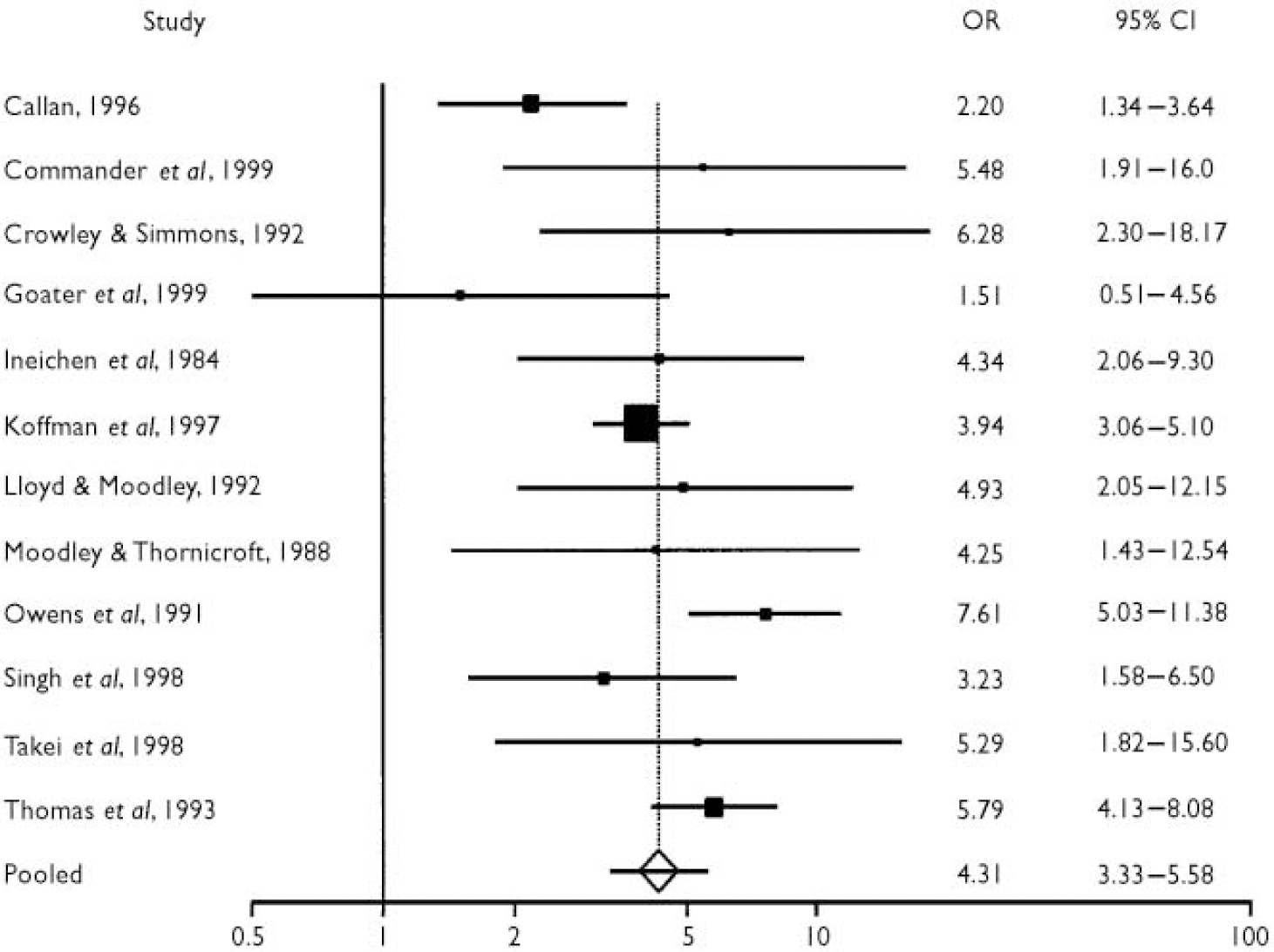
Fig. 1 Odds ratio meta-analysis plot (random effects), Black v. White, from meta-analysis of 12 papers on compulsory admission to in-patient facilities.
DISCUSSION
Main findings
Of many studies addressing any one of our review questions, few actually used the same measure of outcome; therefore, we did not report estimates because, if presented in isolation, these few estimates are likely to give a biased impression. However, the original data tables are available on request and will be posted on the Queen Mary website. Our review suggests that Black people are overrepresented among in-patients, and that Asian patients use in-patient facilities less often than do White patients. Unexpectedly, two papers report an excess of voluntary admissions for White people. There is some evidence for variations in pathways to specialist mental health care, with Black people traversing more complex pathways. Variation in primary care assessments or primary care involvement could explain some of the ethnic differences in pathways to specialist services but the primary care literature is small. Despite concerns about Black people falling out of care, two papers showed that they were more likely to be in contact with services after 5 and 18 years. This could reflect effective delivery of necessary care, or professionals' anxieties about perceived risk. Black people on in-patient units were four times more likely to experience a compulsory admission compared with White people. This is consistent with research in forensic and prison services (Reference Bhui, Brown and HardieBhui et al, 1998; Reference Coid, Kahtan and GaultCoid et al, 2000) and with research informing the proposed amendments of the Mental Health Act. These reported twice the risk (Reference Wall, Churchill and HotopfWall et al, 1999) and six times the risk of compulsory detention of Black people (Reference Audini and LelliottAudini & Lelliott, 2002).
Explaining the findings
No papers reported investigations of discrimination as a risk factor. Perceived discrimination could have a detrimental effect on mental health, placing Black people at higher risk of mental illness and perhaps of mental health service use (Reference Karlsen and NazrooKarlsen & Nazroo, 2002). Perceived discrimination within health care services may further compound this, whereas excessive use of compulsory admission could account for less satisfaction with services and fear of contact with services. Although social isolation (Reference Cole, Leavey and KingCole et al, 1995) can also mediate higher contact with emergency services among Black patients, local variations in clinical practice and service provision are well recognised as sources of inequalities. Most studies did not compare regional variations of clinical practice or service configuration. Most studies were based in London. Even though the majority of the UK's minority ethnic communities live in the largest cities, mental health policy should reflect the needs of regions with smaller proportions of minority ethnic groups. Indeed, recent evidence suggests that contextual effects, such as a lower ethnic density, can actually lead to higher rates of schizophrenia requiring greater service use (Reference Boydell, van Os and McKenzieBoydell et al, 2002).
Methodological considerations
The composition of any one ethnic group varied across the papers. This raises uncertainty about the generalisability of the findings from any single paper to populations that fall within the same ethnic group but have different ethnic subgroup profiles (for example, South Asians with different places of birth, country or region of origin within the Indian subcontinent). Improvement in the quality of the more recent publications is encouraging but the majority did not justify their classification of ethnic groups (Reference Senior and BhopalSenior & Bhopal, 1994) and did not take account of possible variations in service use between subgroups within the larger ethnic categories. Adjustment for socio-economic status did not always relate to study quality, but adjustment for confounders generally and ethnic group definitions did relate to quality.
FUTURE PRIORITIES
Studies including White subgroups and South Asians, services outside of London and community and primary care studies were underrepresented in the literature. Future studies should explore explanations for variations that go beyond assigning all differences to ethnic origins. More-tailored study designs are needed to assess aetio-logical factors, mechanisms to explain ethnic variations and interventions. Where ethnic differences are evident, future investigations should address potential explanatory factors, such as discrimination, practice variation, service configuration and social isolation. Greater attention to place of birth, religion, duration of residence in the UK, place and level of education and cultural identity could also refine the interpretation of data beyond assigning all differences to ethnic origin.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Black patients are more likely to be voluntary or compulsory in-patients.
-
▪ Pathways to specialist services are more complex for Black patients, with more crisis routes of entry into care.
-
▪ Primary care assessments show ethnic variations that could explain some of the variations in specialist service use.
LIMITATIONS
-
▪ We excluded qualitative studies that might shed light on putative mechanisms that explain our findings.
-
▪ The variety of study designs, quality of studies, ethnic group definitions and outcome measures makes comparison, and specifically meta-analyses, inappropriate. This limited the review to a narrative account of differences.
-
▪ There is little information on White subgroups, practice and service variations, South Asian groups, services outside of London and primary care and community services.
APPENDIX
Inclusion and exclusion criteria
Inclusion criteria
Variation studies
UK-based studies, measuring variation in service use or provision for mental health care. Report data for more than one ethnic group, retrospective, prospective or cross-sectional studies of use or provision.
Intervention studies
International studies, including quantitative studies of interventions aiming to improve access and uptake of mental health services by different ethnic groups. The types of interventions could include educational (for users and/or health care professionals), organisational, financial, regulatory. Study designs could include controlled trial, parallel group or before-and-after studies.
Grey/unpublished literature
UK-based data sought from health authorities and by asking three ‘experts’ to identify any major omissions from the identified publications.
Service use
Studies that investigate the rates of use by ethnic groups of facilities provided for mental health care, whether service provision is targeted or non-targeted.
Service provision
Studies were included that investigate provision of services for different ethnic populations and the uptake of these services by their targeted population.
Management of disorders
Drug treatment of any affective or psychotic condition in primary or secondary care.
Participants
Adults identified by ethnic group with an affective or psychotic disorder.
Date of publication
January 1983 to end October 2000.
Language
English, French or German.
Exclusion criteria
Studies of services for children, adolescents, psycho-sexual disorders, substance misuse, alcohol misuse and forensic mental health were excluded.
Acknowledgements
We thank Juliet Formby for carrying out the bibliographic searches, reviewing and coding abstracts and providing administrative support, Alain Besson for designing the search strategies and Marilyn Aviles for contributing to the review protocol and the criteria for judging identification of ethnic groups and reviewing and coding abstracts. For the meta-analysis, we thank Laura Bright for extraction and tabulation data and Helen Tate for performing the analyses.








eLetters
No eLetters have been published for this article.