Despite the fact that dysphoric symptoms represent a significant complicating factor in the successful treatment of bipolar disorder, controlled trials regarding the depressive aspects of acute mania are rare (Reference Montgomery, Schatzberg and GuelfiMontgomery et al, 2000). A post hoc analysis of pooled data from two double-blind, placebo-controlled trials supported the efficacy of olanzapine monotherapy for both manic and depressive aspects of dysphoric mania (Reference Baker, Tohen and FawcettBaker et al, 2003), although the decrease in scores on the Hamilton Rating Scale for Depression (HRSD; Reference HamiltonHamilton, 1967) was driven by improvement in items related to sleep, insight and paranoia. A randomised double-blind, placebo-controlled study demonstrated the efficacy of olanzapine co-therapy in patients with bipolar disorder who had inadequate responses to valproate or lithium monotherapy (Reference Tohen, Chengappa and SuppesTohen et al, 2002). We describe a secondary analysis of data from that study, assessing both depression and manic treatment responses among dysphoric and non-dysphoric patients with bipolar I disorder, who received either olanzapine or placebo in addition to lithium or valproate.
METHOD
Study design
Data were derived from a large, multicentre double-blind study. Patients whose symptoms of mania were partially nonresponsive to 2 weeks of treatment with valproate or lithium monotherapy at therapeutic serum levels were randomised to receive either adjunctive olanzapine (here-after referred to as ‘combination therapy’) or adjunctive placebo (‘monotherapy’) in addition to their existing lithium or valproate monotherapy. We report secondary post hoc analyses focusing on a subgroup of patients with mania or mixed disorder who had substantial comorbid depression at baseline, and examine whether therapeutic response in this ‘dysphoric’ group differed from the remaining ‘non-dysphoric’ patients. The study was conducted at 33 sites in the USA and 5 sites in Canada. Detailed methods and the primary results of this study have been published by Tohen et al (Reference Tohen, Chengappa and Suppes2002).
Patients
The protocol was approved by the institutional review board at each site, and all patients provided written informed consent prior to administration of any study procedures or study medications. At enrolment, all patients had bipolar I disorder as defined by DSM–IV criteria (American Psychiatric Association, 1994), manic or mixed episode, with or without psychotic features, assessed independently of the symptom rating scale scores. Diagnosis was confirmed using the patient version of the Structured Clinical Interview for DSM–IV (SCID–P; Reference First, Spitzer and GibbonFirst et al, 1997). Patients were required to have had at least two previous depressed, manic or mixed episodes, and to have had documented treatment with lithium or valproate for at least 2 weeks prior to visit 1, with a therapeutic blood level of lithium (0.6–1.2 mmol/l) or valproate (50–125 μg/ml) at visit 1. Patients were included in the study only if they showed inadequate response to monotherapy for the 2 weeks prior to randomisation, evidenced by a total score of 16 or more on the Young Mania Rating Scale (YMRS; Reference Young, Biggs and ZieglerYoung et al, 1978). After meeting entry criteria, patients were randomised in a 2:1 ratio to receive either adjunctive olanzapine (flexible daily dosage of 5, 10 or 20 mg) or adjunctive placebo in conjunction with their current valproate or lithium for 6 weeks. Olanzapine was initiated at a daily dosage of 10 mg. Plasma levels of lithium or valproate were documented to be within their therapeutic serum ranges.
Patients were also permitted adjunctive benzodiazepine (≤2 mg daily of lorazepam equivalents) for no more than 14 days cumulatively. Aside from the study drugs, benzodiazepines and anticholinergics (benzatropine mesilate, ≤ 2 mg per day), no other psychotropic drug was permitted during the study.
Assessments
Severity of illness was measured by the 11-item YMRS and the 21-item HRSD. Ratings were completed at baseline and weekly during therapy. The post hoc analysis focused on patients with moderate to severe dysphoric mania, as defined by a baseline HRSD total score of 20 or over. This threshold has been used by others to stratify patients into mild v. moderate to severely ill categories in depression studies (Reference Thase, Greenhouse and FrankThase et al, 1997). Changes in severity of depressive symptoms were assessed using the HRSD total score, HRSD Maier sub-scale and HRSD individual items. The Maier sub-scale comprises six items: item 1 (depressed mood), item 2 (guilt), item 7 (work and activities), item 8 (retardation), item 9 (agitation) and item 10 (psychic anxiety) (Reference Maier, Philipp and GerkenMaier et al, 1985).
Statistical method
Comparisons of baseline demographic and illness characteristics between patients with a baseline HRSD total score of 20 or above and patients with a score below 20 were performed using analysis of variance (ANOVA) with categorisation (dysphoric at baseline/non-dysphoric at baseline) in the model for continuous variables and using Fisher's exact test for categorical variables. Descriptive baseline demographic factors for the olanzapine and placebo treatment groups were also tabulated. The primary efficacy measure was the mean change from baseline to end-point (last observation carried forward up to week 6) for HRSD total score. The ANOVA was performed with treatment, dysphoric/non-dysphoric categorisation and interaction between categorisation and treatment in the model. An additional model with treatment, dysphoric/non-dysphoric categorisation, interaction between categorisation and treatment, mood stabiliser (valproate or lithium) and the interaction between mood stabiliser and categorisation was also explored. The hypothesis that mean improvement in HRSD score in the olanzapine combination therapy group over the placebo monotherapy group did not differ between patients with and without baseline depressive symptoms was tested with the interaction test of dysphoric/non-dysphoric categorisation by treatment. Similar analyses were performed for the YMRS total score. Effect sizes were calculated as the difference between combination therapy and monotherapy divided by the estimated standard deviation obtained from the square root of the mean square error of the ANOVA model.
To evaluate the time course of improvement, a mixed-model repeated measures (MMRM) analysis of variance was fitted for change from baseline in HRSD total score with investigator, treatment, visit, visit–treatment interaction, dysphoric categorisation (dysphoric v. non-dysphoric), dysphoric categorisation–treatment and dysphoric categorisation–visit and the three-way interaction of dysphoric categorisation–treatment–visit. An unstructured covariance matrix was fitted to the within-patient repeated measures. Using contrasts within the repeated measures model, the main overall effect of treatment within each dysphoric subgroup was assessed, as was the change from baseline to each visit between treatment groups.
Patients were analysed on an intention-to-treat basis for all analyses. Patients with a baseline assessment and at least one post-baseline measurement were included in the analysis. The YMRS and HRSD total scores were derived from the individual items; if any single item was missing, the total score was treated as missing. All P values were based on two-tailed tests with a significance level of 0.05.
RESULTS
Patients
Baseline patient and illness characteristics by dysphoric/non-dysphoric categorisation and treatment group are summarised in Table 1. Of 344 randomised patients, 85 met the study criterion for dysphoric mania (olanzapine combination treatment, n=60; placebo monotherapy, n=25) and 259 for non-dysphoric mania (combination treatment, n=169; monotherapy, n=90). Within the dysphoric subgroup, 84.7% of patients met DSM–IV criteria for a mixed episode. The dysphoric and non-dysphoric groups contained similar proportions of patients being treated with valproate (70.6% and 64.3% respectively, P=0.356) and lithium (29.4% and 35.7% respectively). Mean modal dose of olanzapine did not differ significantly between dysphoric and non-dysphoric patients (11.4 mg v. 10.0 mg; P=0.15).
Table 1 Baseline patient and illness characteristics

| Characteristic | Baseline dysphoric mood1 | No baseline dysphoric mood1 | P 4 | ||||
|---|---|---|---|---|---|---|---|
| Combination therapy2 (n=60) | Monotherapy3 (n=25) | Total (n=85) | Combination therapy2 (n=169) | Monotherapy3 (n=90) | Total (n=259) | ||
| Age, years: mean (s.d.) | 38.16 (10.33) | 40.28 (11.20) | 38.78 (10.57) | 41.64 (11.44) | 40.46 (10.78) | 41.23 (11.20) | 0.077 |
| Gender | |||||||
| Male (%) | 37 | 28 | 34 | 47 | 63 | 53 | 0.004 |
| Ethnicity | |||||||
| White (%) | 82 | 96 | 86 | 87 | 81 | 85 | 1.000 |
| Episode type | |||||||
| Mixed (%)5 | 85 | 84 | 85 | 44 | 37 | 41 | <0.001 |
| Psychotic features present (%)6 | 48 | 36 | 45 | 27 | 33 | 29 | 0.012 |
| Rapid cycling (%)7 | 52 | 40 | 48 | 42 | 48 | 44 | 0.531 |
| Mood stabiliser | |||||||
| Valproate (%) | 63 | 88 | 71 | 68 | 57 | 64 | 0.356 |
| Previous depression lifetime episodes (%) | |||||||
| ≤ 2 | 10 | 12 | 11 | 26 | 25 | 26 | 0.0018 |
| 3–10 | 30 | 44 | 34 | 36 | 27 | 33 | |
| 11–50 | 20 | 12 | 18 | 19 | 26 | 22 | |
| > 50 | 40 | 32 | 38 | 19 | 23 | 20 | |
| Previous mania lifetime episodes (%) | |||||||
| ≤ 2 | 13 | 16 | 14 | 20 | 13 | 18 | 0.0118 |
| 3–10 | 22 | 44 | 28 | 32 | 37 | 34 | |
| 11–50 | 23 | 4 | 18 | 25 | 19 | 23 | |
| > 50 | 42 | 36 | 40 | 22 | 31 | 25 | |
| Previous mixed lifetime episodes (%) | |||||||
| ≤ 2 | 22 | 32 | 25 | 46 | 47 | 47 | <0.0018 |
| 3–10 | 20 | 20 | 20 | 21 | 13 | 18 | |
| 11–50 | 15 | 8 | 13 | 12 | 16 | 13 | |
| > 50 | 42 | 40 | 42 | 20 | 25 | 22 | |
| YMRS total score, mean (s.d.) | 23.80 (5.16) | 23.24 (4.65) | 23.64 (4.99) | 21.81 (5.33) | 22.57 (5.30) | 22.07 (5.32) | 0.018 |
| HRSD total score, mean (s.d.) | 25.33 (4.82) | 24.60 (4.12) | 25.18 (4.62) | 10.44 (5.39) | 10.39 (5.06) | 10.42 (5.27) | <0.001 |
Efficacy: depressive symptoms
For the analysis of change in HRSD total score from baseline to end-point, the interaction between mood stabiliser (valproate or lithium) and dysphoric categorisation was not significant (P=0.290), indicating that the treatment effect of olanzapine combination therapy over monotherapy was not dependent upon whether patients were taking valproate or lithium. In addition, the main effect of mood stabiliser was also not significant (P=0.528), indicating that change in HRSD score did not differ in patients taking valproate v. those taking lithium. Since these two terms were not statistically significant, they were dropped from the model for the analysis of HRSD total score as well as the HRSD Maier sub-scale and individual items.
For the HRSD total score, there was a statistically significant interaction between categorisation (baseline dysphoric/non-dysphoric) and treatment group (P=0.016), indicating that mean HRSD score improvement in combination therapy patients over monotherapy patients differed between those with and without baseline dysphoria (Table 2). In both dysphoric and non-dysphoric patients, improvement in HRSD total score was significantly greater for patients receiving combination therapy compared with monotherapy (dysphoric group –8.82 v. – 1.42, P<0.001; non-dysphoric group –2.87 v. 0.01, P=0.002). However, the magnitude of the difference between combination and monotherapy treatment groups was larger for the dysphoric patients (Fig. 1), thus driving the significant interaction. The difference between treatment groups is also apparent from a comparison of effect sizes for the dysphoric patients (1.11) with that of non-dysphoric patients (0.43).
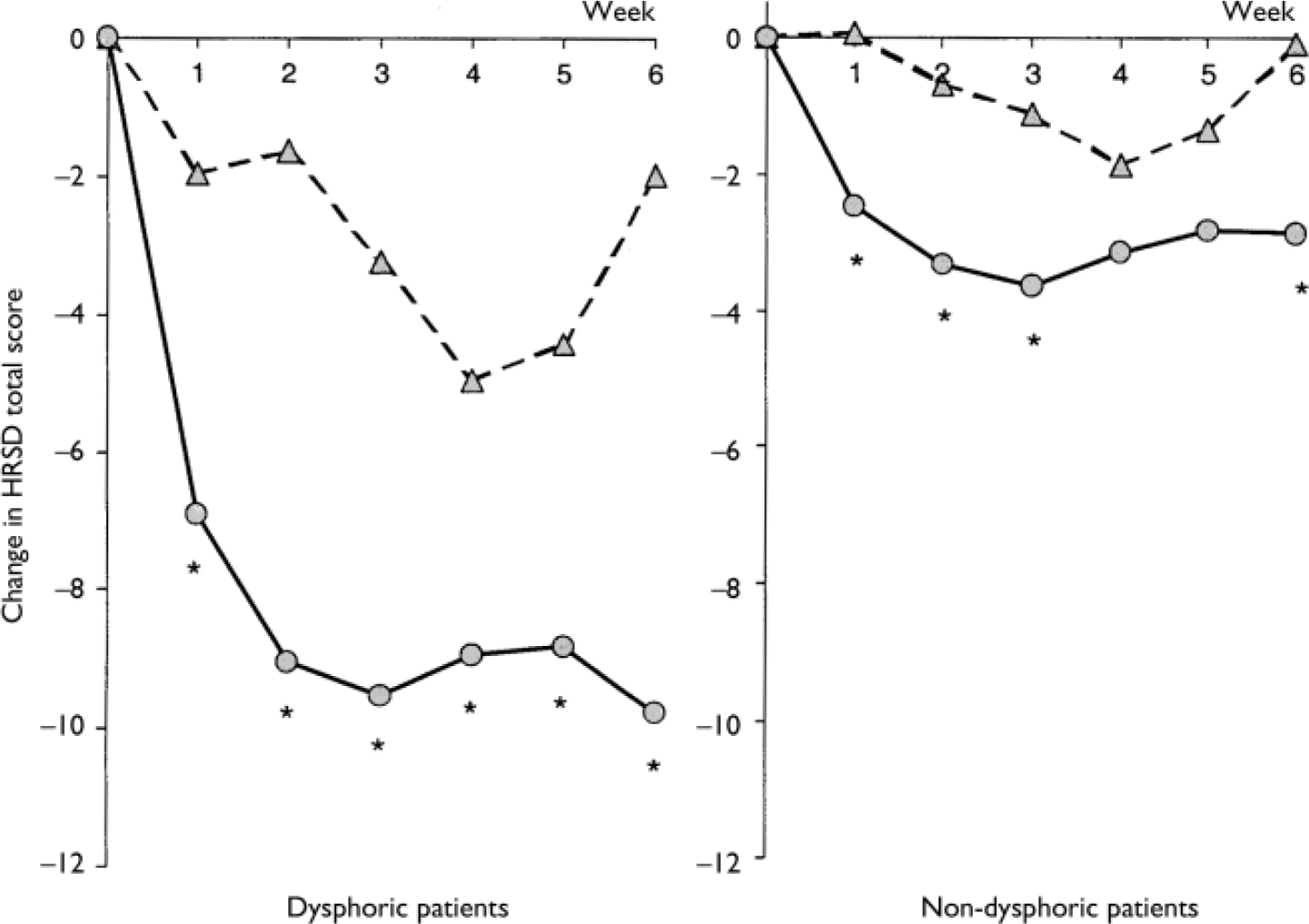
Fig. 1 Mean change in Hamilton Rating Scale for Depression (HRSD) total score for dysphoric patients (left-hand graph) and non-dysphoric patients (right-hand graph) receiving olanzapine plus lithium or valproate (combination therapy; circles) or placebo plus lithium or valproate (monotherapy; triangles). Dysphoric patients: combination therapy n=60, monotherapy n=25; non-dysphoric patients: combination therapy n=169, monotherapy n=90; *, P<0.01v. placebo.
Table 2 Summary of efficacy measures: least square means from analysis of variance model

| Item | Interaction1 | Dysphoric patients | Non-dysphoric patients | ||||||
|---|---|---|---|---|---|---|---|---|---|
| P | Combination therapy2 | Monotherapy3 | P 4 | Effect size | Combination therapy2 | Monotherapy3 | P 4 | Effect size | |
| HRSD | |||||||||
| Total | 0.016 | – 8.82 | – 1.42 | <0.001 | 1.11 | – 2.87 | 0.01 | 0.002 | 0.43 |
| Maier sub-scale | 0.556 | – 2.73 | – 0.45 | 0.013 | 0.61 | – 1.07 | 0.59 | 0.001 | 0.45 |
| Individual items | |||||||||
| 1 Depressed mood | 0.817 | – 0.31 | 0.15 | 0.111 | 0.39 | – 0.04 | 0.50 | <0.001 | 0.45 |
| 2 Feelings of guilt | 0.950 | – 0.55 | – 0.14 | 0.065 | 0.45 | – 0.34 | 0.09 | <0.001 | 0.47 |
| 3 Suicide | 0.016 | – 0.45 | 0.15 | 0.001 | 0.80 | 0.07 | 0.16 | 0.361 | 0.12 |
| 4 Insomnia (early) | 0.048 | – 0.90 | – 0.18 | 0.003 | 0.73 | – 0.33 | – 0.16 | 0.182 | 0.18 |
| 5 Insomnia (middle) | <0.001 | – 0.89 | 0.09 | <0.001 | 1.13 | – 0.45 | – 0.33 | 0.322 | 0.13 |
| 6 Insomnia (late) | 0.040 | – 0.75 | – 0.16 | 0.005 | 0.69 | – 0.35 | – 0.25 | 0.416 | 0.11 |
| 7 Work and activities | 0.933 | – 0.38 | – 0.27 | 0.686 | 0.12 | – 0.02 | 0.12 | 0.367 | 0.14 |
| 8 Retardation | 0.333 | – 0.10 | 0.07 | 0.275 | 0.27 | 0.18 | 0.17 | 0.960 | – 0.01 |
| 9 Agitation | 0.631 | – 0.76 | – 0.41 | 0.181 | 0.33 | – 0.56 | – 0.36 | 0.158 | 0.19 |
| 10 Anxiety (psychic) | 0.152 | – 0.63 | 0.15 | 0.003 | 0.74 | – 0.30 | 0.05 | 0.013 | 0.34 |
| 11 Anxiety (somatic) | 0.322 | – 0.50 | – 0.17 | 0.132 | 0.37 | – 0.14 | – 0.06 | 0.512 | 0.09 |
| 12 Somatic symptoms (GI) | 0.031 | – 0.42 | – 0.09 | 0.008 | 0.65 | – 0.11 | – 0.09 | 0.775 | 0.04 |
| 13 Somatic symptoms (general) | 0.992 | – 0.12 | – 0.02 | 0.584 | 0.13 | 0.02 | 0.13 | 0.314 | 0.14 |
| 14 Genital symptoms | 0.110 | – 0.15 | 0.14 | 0.121 | 0.38 | 0.07 | 0.02 | 0.594 | – 0.07 |
| 15 Hypochondriasis | 0.412 | – 0.49 | – 0.30 | 0.266 | 0.27 | 0.02 | 0.04 | 0.768 | 0.04 |
| 16 Loss of weight | 0.565 | 0.00 | 0.13 | 0.128 | 0.37 | – 0.01 | 0.06 | 0.122 | 0.21 |
| 17 Insight | 0.845 | 0.03 | – 0.04 | 0.590 | – 0.13 | – 0.08 | – 0.12 | 0.573 | – 0.08 |
| 18 Diurnal variation | 0.237 | – 0.35 | – 0.43 | 0.653 | – 0.11 | – 0.09 | 0.06 | 0.099 | 0.22 |
| 19 Depersonalisation and derealisation | 0.517 | – 0.38 | – 0.29 | 0.516 | 0.16 | 0.01 | 0.00 | 0.858 | – 0.02 |
| 20 Paranoid symptoms | 0.217 | – 0.53 | 0.03 | 0.002 | 0.75 | – 0.32 | – 0.02 | 0.003 | 0.40 |
| 21 OC symptoms | 0.233 | – 0.11 | 0.16 | 0.033 | 0.52 | – 0.11 | – 0.02 | 0.171 | 0.19 |
| YMRS Total | 0.111 | – 11.75 | – 4.65 | <0.001 | 0.84 | – 13.06 | – 9.78 | 0.005 | 0.39 |
A significant interaction existed between treatment and dysphoric subgroup, indicating that treatment group differences were dependent upon patients' dysphoric status (dysphoric v. non-dysphoric). Furthermore, MMRM analysis detected a significant interaction between treatment and visit, indicating that the response over time differed between the treatment groups (P=0.009). Plots of changes in mean HRSD total scores over time for dysphoric and non-dysphoric subgroups are presented in Fig. 1. For each subgroup, an overall treatment difference was detected (olanzapine combination therapy superior to monotherapy; P<0.001 in both cases) and this difference was observed as early as the first post-randomisation visit (week 1).
Analysis of the HRSD Maier sub-scale revealed no significant interaction between dysphoric categorisation and treatment, indicating that the beneficial effect of combination therapy over monotherapy was similar in dysphoric and non-dysphoric patients. In both groups, improvement in Maier sub-scale score was significantly greater for patients receiving olanzapine combination therapy than for those receiving monotherapy (dysphoric group –2.73 v. –0.45, P=0.013; non-dysphoric group –1.07 v. 0.59, P=0.001).
Statistically significant interactions between dysphoric categorisation and treatment were observed for five HRSD individual items (Table 2). For each of these five items, dysphoric patients receiving olanzapine combination therapy demonstrated significantly superior improvement over those receiving monotherapy, corresponding to large effect sizes. In contrast, patients in the non-dysphoric category exhibited no significant difference for these five items and small effect sizes between treatment groups. In the case of item 10 (psychic anxiety), significant between-treatment differences were observed in both dysphoric and non-dysphoric patient groups. For HRSD items 1 (depressed mood) and 2 (feelings of guilt), effect sizes were approximately 0.45 for both subgroups – however, significant treatment differences were only seen in the non-dysphoric group, possibly owing to the smaller size of the dysphoric group. In the case of HRSD items 20 (paranoid symptoms) and 21 (obsessional and compulsive symptoms), significant differences were detected between combination and monotherapy in the dysphoric patient group, whereas in the non-dysphoric group there was a significant difference between treatment groups for item 20 only.
Efficacy: manic symptoms
Analysis of YMRS total score revealed no significant interaction between mood stabiliser (valproate or lithium) and treatment, or in the main effect of mood stabiliser (P>0.20 for both), indicating that the difference in treatment group response was not dependent upon whether patients were receiving valproate or lithium. Furthermore, no statistically significant interaction existed between dysphoric/non-dysphoric categorisation and treatment (P=0.111; Table 2), indicating that improvements in mania severity for combination therapy over monotherapy were independent of dysphoric/non-dysphoric categorisation. Statistically significant differences were detected between treatment groups for both dysphoric and non-dysphoric categories. The difference between treatment groups was numerically (although not significantly) larger for the dysphoric patients (interaction P=0.111). However, this was due primarily to a larger monotherapy response among non-dysphoric patients (mean change for dysphoric patients – 4.65 v. non-dysphoric patients –9.78; P=0.013) rather than a significant difference in combination treatment response between groups (mean change for dysphoric patients –11.75 v. non-dysphoric patients –13.06; P=0.361).
DISCUSSION
This analysis found that olanzapine therapy combined with either valproate or lithium effectively treated coexisting manic and depressive symptoms in patients who experienced inadequate response or breakthrough symptoms during lithium or valproate monotherapy. Patients receiving combination treatment demonstrated significantly greater improvement compared with those receiving monotherapy in depressive symptom severity (HRSD total score). A substantial proportion of the treatment benefits in depression occurred within core mood symptoms. Significant improvements were also observed in mania symptom severity (YMRS total score) in the combination therapy group compared with the monotherapy group.
Although defined rather differently, the terms ‘dysphoric mania’, ‘depressive mania’ and ‘mixed mania’ are used somewhat interchangeably, as each describes a manic episode complicated by prominent comorbid depressive features (Reference Bauer, Whybrow and GyulaiBauer et al, 1994; Reference Akiskal, Hantouche and BourgeoisAkiskal et al, 1998; Reference Dilsaver, Chen and ShoaibDilsaver et al, 1999; Reference Perugi, Akiskal and MicheliPerugi et al, 2001). Given that patients experiencing these dysphoric manic episodes are reported to constitute up to two-thirds of bipolar disorder clinical samples (Reference Akiskal, Bourgeois and AngstAkiskal et al, 2000), it might be expected that effective treatment options would exist. However, the overall prognosis for patients with dysphoric mania is worse than for those with pure mania (Reference Himmelhoch and GarfinkelHimmelhoch & Garfinkel, 1986; Reference Keller, Lavori and CoryellKeller et al, 1986; Reference Secunda, Swann and KatzSecunda et al, 1987), and in fact our data at baseline (see Table 1) indicate greater severity of many variables in the dysphoric group.
A key treatment challenge in bipolar disorder, especially among patients with mixed mania and rapid cycling, is to bring about improvement of symptoms of one mood pole without worsening or accelerating the onset of symptoms of the opposite pole. Ideally, one medication would be employed to treat both mood symptom poles simultaneously. However, so far controlled monotherapy studies have failed to demonstrate that this goal has been achieved, especially in mixed or dysphoric mania. Among the classic mood stabilisers, the body of evidence suggesting antidepressant effects during lithium monotherapy is much less robust than that supporting its antimanic properties, and valproate may be preferable to lithium in the treatment of dysphoric mania (Reference McElroy, Keck and PopeMcElroy et al, 1988; Reference Freeman, Clothier and PazzagliaFreeman et al, 1992; Reference Swann, Bowden and MorrisSwann et al, 1997). For valproate, evidence of efficacy is stronger for manic features than for depressive features of dysphoric mania (Reference Swann, Bowden and MorrisSwann et al, 1997). Olanzapine's antimanic properties are well established (Reference Tohen, Jacobs and GrundyTohen et al, 2000). In addition, olanzapine appears to reduce symptoms of bipolar depression, albeit less effectively when given alone than in combination with fluoxetine (Reference Tohen, Vieta and CalabreseTohen et al, 2003a ). In an earlier study we described the efficacy of olanzapine monotherapy in treating both manic and depressive symptoms in dysphoric and non-dysphoric in-patients (Reference Baker, Tohen and FawcettBaker et al, 2003). Olanzapine demonstrated significant improvement in YMRS total score compared with placebo in both dysphoric and non-dysphoric patients, and also produced significant improvement in HRSD total score in the dysphoric group (Reference Baker, Tohen and FawcettBaker et al, 2003). This is to our knowledge the only previous placebo-controlled demonstration of simultaneous improvement in depressive and manic symptoms of dysphoric mania during treatment with a single agent. Further study seemed appropriate, however, given that the previous report had important limitations, such as small sample size and non-statistically significant improvement in Maier sub-scale scores.
Our analysis includes effect size calculations. An effect size of 1.0 reflects difference between treatment groups of the same magnitude as 1 standard deviation within the population. This can be translated into a probability statement that indicates that the improvement in score of an average individual in the comparison group exceeds that of 84% of patients in the placebo group. Effect size is a useful tool for comparing findings across studies, and by convention an effect size of 0.2 is considered small, 0.5 moderate and 0.8 or greater large (Reference CohenCohen, 1988). This study demonstrated a large effect size (1.11) for improvement of depression in patients with baseline dysphoria who received olanzapine in addition to lithium or valproate. Whereas our previous report did not demonstrate clear benefit in terms of Maier core mood sub-scale, this study demonstrated a moderate effect size for this sub-scale (0.61).
Our analyses have several limitations. First, these are post hoc analyses of data from a clinical trial which evaluated severity of manic symptoms (YMRS total score) as the primary efficacy measure. Second, assignment to valproate or lithium was not randomised but reflected the treatment preferences of clinicians and investigators. Third, the study design lacked an olanzapine monotherapy arm, which makes it difficult to draw any conclusions regarding the relative contributions of olanzapine alone, or synergistic effects with the concomitant medication, to the overall treatment benefits. In fact, no inference can be drawn regarding the relative merit of other treatments or combinations that were not evaluated in this trial. For example, improvement on classical antipsychotic agents would be of interest, given that a recent mania treatment comparison of olanzapine and haloperidol did not establish differential treatment response of depressive symptoms among the small (n=19) subgroup with baseline HRSD scores of 20 or over (Reference Tohen, Goldberg and Gonzalez-Pinto ArrillagaTohen et al, 2003b ). Fourth, the high proportion of participants in rapid-cycling disorder is notable. A rapid-cycling course may affect mania phenomenology – for example, some ‘dysphoric’ patients may be in transition from mania to depression (Reference Kraepelin, Robertson and BarclayKraepelin, 1921; Reference Himmelhoch, Mulla and NeilHimmelhoch et al, 1976; Reference McElroy, Keck and PopeMcElroy et al, 1992) – and its relationship to dysphoric mania is unclear (Reference Himmelhoch, Mulla and NeilHimmelhoch et al, 1976; Reference Post, Rubinow and UhdePost et al, 1989; Reference McElroy, Keck and PopeMcElroy et al, 1992). Finally, the subject group of interest (patients with a baseline HRSD total score of 20 or above) was not defined a priori. In this study most dysphoric patients were diagnosed with mixed episodes, but interestingly there was imperfect homology between a DSM–IV mixed mania diagnosis and dysphoric mania as defined by rating scales. The DSM–IV definition of a mixed manic phase requires patients to simultaneously meet criteria for both a major depressive episode and a manic episode. However, some argue that a DSM–IV syndromal approach may not be optimal for identifying patients with mania and clinically important comorbid depressive features (Reference Cassidy, Murry and ForestCassidy et al, 1998; Reference Cassidy and CarrollCassidy & Carroll, 2001; Reference Dilsaver, Chen and ShoaibDilsaver et al, 1999), and a number of proposals have been put forward which attempt to provide a framework within which a diagnosis of dysphoric mania may be made (Reference McElroy, Keck and PopeMcElroy et al, 1992; Reference Perugi, Akiskal and MicheliPerugi et al, 1997; Reference Cassidy, Ahearn and MurryCassidy et al, 2000; Reference Akiskal, Azorin and HantoucheAkiskal et al, 2003). These proposals require the presence of a full manic episode, plus the presence of two or three defined depressive symptoms. For the purpose of this study, in which all patients met criteria for a manic episode, we used a threshold HRSD total score of 20 or over to define a group of patients displaying prominent depressive features. We believe that this use of an objective rating scale represents a clinically meaningful approach to identifying subjects. In the context of this clinical trial, the DSM–IV and HRSD categorisation systems are somewhat incongruent, with approximately twice the number of patients being identified as ‘mixed’ as were categorised as dysphoric based on symptom ratings. One potential contribution to the incongruence is that symptom ratings coincided with treatment randomisation, whereas diagnostic verification could have taken place up to a week prior to randomisation. In any case, the dysphoric subgroup primarily included patients with diagnosis of a mixed episode.
In conclusion, our analyses found that olanzapine in combination with either lithium or valproate was effective in improving the severity of depressive symptoms coexisting with acute mania. Furthermore, olanzapine co-therapy with lithium or valproate also demonstrated efficacy in the management of manic symptoms, irrespective of whether such symptoms were complicated by concurrent dysphoria. Given the prognostic implications of dysphoric features in mania, and the limited number of pharmacological options currently available for such patients, prospectively designed studies of combination therapy with mood stabilisers and typical antipsychotics in the management of dysphoric mania are encouraged. Such studies should consider innovative strategies for defining dysphoric mania that transcend the limited perspective of DSM–IV mixed states (Reference Perugi, Akiskal and MicheliPerugi et al, 1997; Reference Akiskal, Azorin and HantoucheAkiskal et al, 2003).
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Although dysphoric symptoms represent a significant complicating factor in the successful treatment of bipolar disorder, current treatment options are limited.
-
▪ In this study, olanzapine in combination with either lithium or valproate was effective in improving the severity of depressive symptoms coexisting with acute mania.
-
▪ Olanzapine co-therapy also demonstrated efficacy in managing manic symptoms, irrespective of the presence of concurrent dysphoria.
LIMITATIONS
-
▪ The study used post hoc analysis of data from a clinical trial which evaluated mania rating scale score as the primary efficacy measure.
-
▪ Assignment to valproate or lithium therapy was not randomised but reflected the treatment preferences of clinicians and investigators.
-
▪ The study did not include a typical antipsychotic comparator.
Acknowledgement
This work was supported by Lilly Research Laboratories.








eLetters
No eLetters have been published for this article.