The reduction of the prevalence of depression is a major challenge for public mental health (World Health Organization, 2001). Despite recent clinical developments, the prevalence of depression in European countries has not fallen in recent years (Reference Andrews, Sanderson and SladeAndrews et al, 2000). Problems have included reluctance to consult primary care doctors and the limited capacity of psychological services. In the UK, large-scale psycho-educational stress workshops set up to provide an accessible and brief intervention for anxiety (Reference Brown, Cochrane and HancoxBrown et al, 2000) were shown to be effective and to reach many who had not previously consulted their general practitioners. However, when similar psycho-educational depression workshops were run, they attracted relatively few people, of whom most had already been referred to specialist services (Reference Watkins, Elliott and StanhopeWatkins et al, 2000). Consequently, new workshops were developed, entitled ‘How to improve your self-confidence’. This preliminary study examines the success of these workshops in attracting depressed members of the local population and assesses their efficacy, using a randomised controlled design.
METHOD
Self-confidence workshops
A series of day-long self-confidence workshops for up to 25 people was run in an area of south-east London, with a population of over 1 million people, with the aim of helping participants improve their self-confidence and so reduce their depression, given the link between depression and low self-esteem (Reference Beck, Rush and ShawBeck et al, 1979). Publicity material was distributed over a period of 3 months to health centres, leisure centres, community centres and libraries, inviting people interested in attending these workshops to telephone for further information. No exclusion criterion was used.
The workshops were free and took place on a Sunday to reduce the possibility of work or domestic arrangements affecting attendance. To reduce the possibility of stigmatisation, and consequent reluctance to seek help (Reference Hayward and BrightHayward & Bright, 1997), they were held in a leisure centre rather than a mental health care setting. The workshops began in October 2001. All individuals who enquired were invited to an introductory talk which gave further information about the workshop process and an opportunity to participate in the study.
Up to 25 people could attend each of the workshops, which were run by two clinical psychologists and two assistant psychologists. The programme started at 09.30 h and finished at 16.30 h, with refreshment breaks. The workshops used cognitive-behavioural techniques adapted into an educational programme based on previous workshop programmes and on Fennell's book Overcoming Low Self-esteem (Reference FennelFennel, 1999). The main aim of the programme was to help participants understand problems of low self-confidence and to teach them techniques of improving their self-confidence and self-esteem.
The day's programme was structured into four sessions. In the first session, information was given about the development of low self-confidence and its emotional aspects, including depression. The second session consisted of cognitive aspects of low self-confidence, specifically identifying and challenging negative thoughts. Behavioural methods for improving low self-confidence, including problem-solving and assertiveness, were taught in the third session. The final session was devoted to action planning, with participants setting their own homework targets to start improving their confidence. To reduce the possibility of participants becoming bored or tired, training methods were varied and included didactic sections, large-group exercises, role-play demonstrations and discussions of vignettes of people with low self-confidence.
Three months after each workshop, a 2 h follow-up meeting was organised for participants to complete the self-assessment forms, report on their progress and discuss any problems.
Study design
A randomised controlled trial design was used to evaluate the efficacy of the self-confidence workshops. The 3-month outcomes of people attending a workshop were compared with those of a control group waiting to attend one. The design can be summarised as two group × two time periods with repeated measures on the time variable. It was predicted that the workshops would lead to lower depression and increased self-esteem among workshop participants compared with the people on the waiting list. In addition, it was predicted that self-confidence workshops would be more likely than the ‘Coping with depression’ workshops (Reference Watkins, Elliott and StanhopeWatkins et al, 2000) to attract people who had depressive problems but who might not have consulted their general practitioner. This hypothesis was tested using specific items in the initial questionnaire given to all participants. One question was ‘Have you ever seen your GP about your depression?’ A similar question was asked in relation to anxiety.
Procedure
Consent and baseline data were collected at the introductory talk. Participants were each given a unique identifier and were randomly allocated, using computerised random numbers, to experimental and control groups. A research worker who was not part of the clinical team carried out the randomisation process and informed participants by post of the workshop to which they had been allocated. The experimental workshops took place 2-3 weeks after the introductory talks, and the control workshops took place after 3 months. Participants in the experimental group completed assessments at the introductory talks and at 3-month follow-up. Those who did not attend the follow-up meeting were sent the assessment forms and asked to return them in pre-addressed envelopes. Control participants were asked to complete assessments at the introductory talk and again 3 months later, during a half-hour period immediately before the start of their workshop. Two experimental and two control workshops were run. Each participant attended only one workshop.
Measures
Socio-demographic details and information about past contact with psychiatric and primary care services were recorded on the initial self-report questionnaire. Outcome variables were:
-
(a) the Beck Depression Inventory (BDI; Reference Beck, Ward and MendelsonBeck et al, 1961): scores were categorised into mild depression (10-18), moderate/severe depression (19-29) and extremely severe depression (30-63); scores below 10 indicated no depression;
-
(b) Spielberger's State-Trait Anxiety Inventory (STAI; Reference Spielberger, Gorsuch and LushensSpielberger et al, 1970): this assesses temporary state (STAI-S) and more stable trait (STAI-T) anxiety;
-
(c) the 12-item General Health Questionnaire (GHQ-12; Reference Goldberg and WilliamsGoldberg & Williams, 1988): a cut-off score of 3 or more was used to indicate a ‘probable case’;
-
(d) the Rosenberg Self-Esteem Scale (RSES; Reference RosenbergRosenberg, 1965).
Analyses
Data were analysed using a two-way analysis of variance with repeated measures. A power calculation using a two-tailed significance level of 0.05 to achieve 80% power in a two-group comparison indicated that a sample size of 64 in each group is needed for a medium effect size of 0.5. Categorical data were analysed using the chi-squared test.
RESULTS
A total of 134 people attended the introductory talks and 120 agreed to participate in the study (Fig. 1). This represents an initial refusal rate of 10.4%. Of the 60 people allocated to the experimental group, 44 (73%) attended their assigned workshop and 40 of these participants were successfully followed up. In the control group, 39 (65%) attended their assigned workshop.
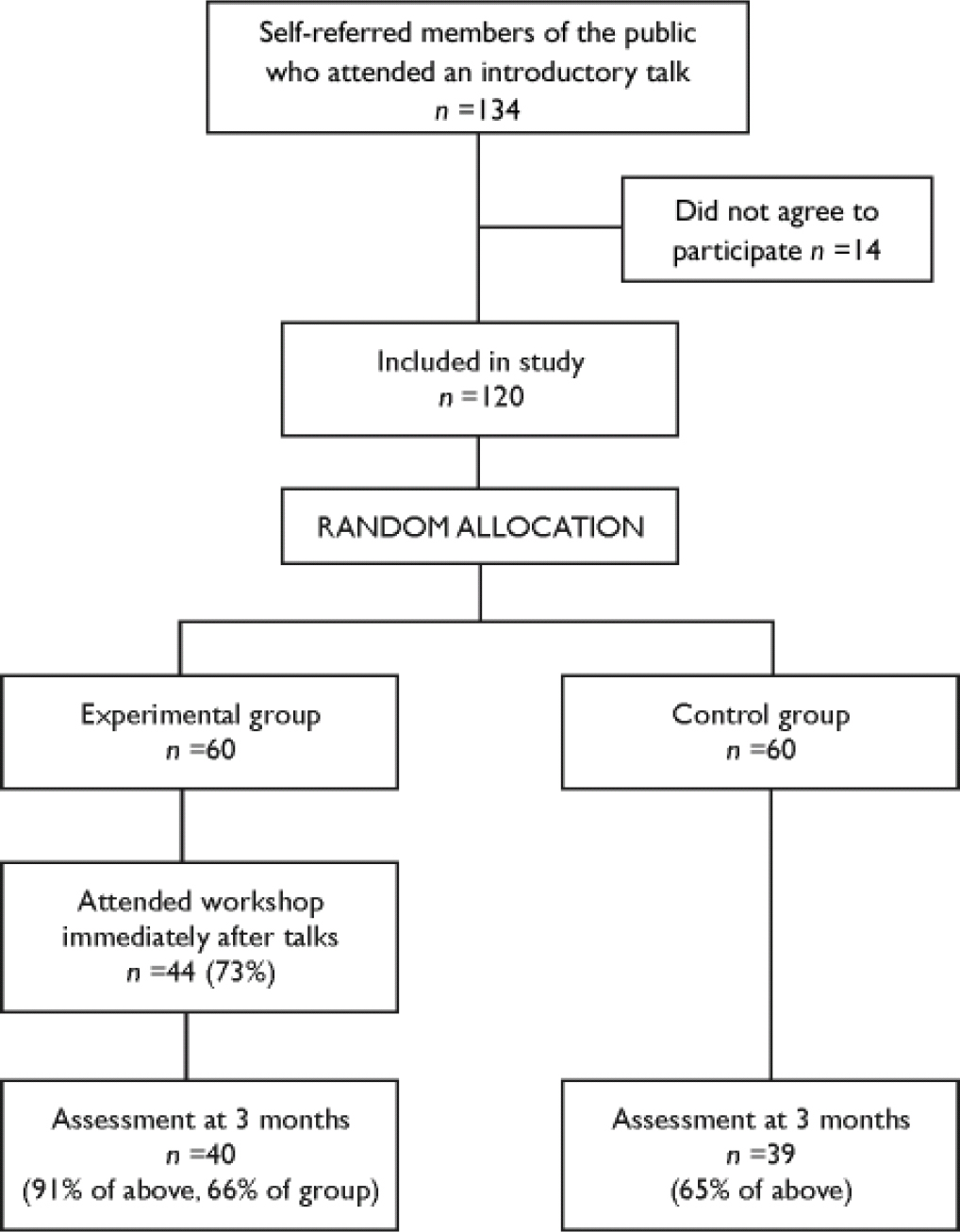
Fig. 1 Flow of participants through the study.
Demographic details
Compared with the general population in the area, those who attended the introductory talks were much more likely to be female (83%), aged 35-44 years (35%) and single (46%). They were, however, reasonably representative in employment status (58% employed, 14% unemployed and 31% unoccupied, e.g. retired or studying) and ethnic origin (61% White, 22% Black and 5% Asian). Occupational classes II (28%) and III (non-manual) (36%) were overrepresented; class IV (8%) was representative of the local population; and classes I (2%), III (manual) (7%), V (1%) and the ‘unoccupied’ category (19%) were underrepresented.
Previous treatment
Data on previous consultation for depression were missing for 8 participants. Of the remaining 112 participants, 44 (39%) had never consulted their general practitioner about their depression and 72 (64%) had not done so in the previous 3 months. This contrasts with 90.2% (37 out of a total of 41 participants) who had already consulted their general practitioner when they referred themselves to the ‘Coping with depression’ workshops (Reference Watkins, Elliott and StanhopeWatkins et al, 2000). Thus it appears that changing the title of the workshop from ‘Depression’ to ‘Self-confidence’ attracted more people who had not sought medical help.
Severity of problems
Three-quarters of the 120 participants had GHQ-12 scores of 3 or above. Depressive problems were most commonly reported as recurrent (58%) and lasting over 5 years (41%). Categorised by BDI score, 31% (n=37) had mild depression, 37% (n=44) had moderate/severe depression and 18% (n=21) had extremely severe depression. Of the 15% (n=18) who scored below 10 and did not have current depression, almost half (n=8) said that they had experienced recurrent anxiety problems for over a year and more than a quarter (n=5) said they had had depressive problems for over 5 years.
Severity of problems and consultation for depression
A further analysis of the 112 participants for whom data were available showed that those who had consulted their general practitioner had significantly higher GHQ-12 scores (mean 7.5) compared with those who had not consulted (mean 5.16; t=2.99, d.f.=110, P<0.01). Of the 39% (n=44) of participants who had not previously consulted their general practitioner, 70 (n=31) had current depression, with a mean BDI score of 20.26. The 13 participants who scored below 10 on the BDI (mean 5.23) and who had not consulted appeared to have some anxiety problems, as they had a mean score of 39.23 on the STAI-T scale. Table 1 shows an analysis of consultation according to the severity of depression.
Table 1 Previous consultation of general practitioner for depression, categorised by severity of depression (n=112)
| BDI score | Previously consulted GP n (%) | Did not previously consult n (%) |
|---|---|---|
| No depression (0–9) | 4 (6) | 13 (30) |
| Mild depression (10–18) | 16 (24) | 18 (41) |
| Moderate/severe depression (19–29) | 32 (47) | 8 (18) |
| Extremely severe depression (30–63) | 16 (24) | 5 (11) |
| Total | 68 | 44 |
Evaluation of intervention
The experimental and control groups did not differ in background socio-demographic details or scores at baseline. Table 2 shows the baseline and outcome scores for the 79 participants who completed the 3-month assessment, and the results of the analyses, which showed significantly superior outcomes on the BDI, GHQ-12 and RSES for the experimental group, as indicated by group × time interactions. No other group × time interaction was significant. Changes in BDI score of at least 10 points were used to indicate clinically significant improvement, and by this criterion 45% of the experimental group improved compared with 8% of the control group (χ2=14.1, d.f.=1, P<0.001).
Table 2 Scores of experimental and control groups at baseline and at 3-month follow-up
| Measure | Experimental group (n=40) | Control group (n=39) | Two-way ANOVA (F values) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline score | Follow-up score | Baseline score | Follow-up score | Group | Time | Group × time | |||||||||
| Mean | s.d. | 95% CI | Mean | s.d. | 95% CI | Mean | s.d. | 95% CI | Mean | s.d. | 95% CI | ||||
| BDI | 21.87 | 11.3 | 18.7–25 | 13.1 | 10.3 | 10–16 | 17.38 | 8.99 | 14–20.6 | 16 | 8.44 | 13–19 | 0.157 | 29.21**** | 15.47**** |
| GHQ–12 | 6.5 | 4.42 | 5.2–7.8 | 3.05 | 3.83 | 1.8–4.3 | 6.11 | 4.03 | 4.7–7.4 | 4.83 | 3.93 | 3.6–6 | 0.85 | 20.1*** | 4.28* |
| RSES | 16.55 | 8.35 | 14–19 | 20.75 | 8.43 | 18–23.3 | 18.32 | 7.56 | 15.7–20.9 | 18.47 | 7.88 | 15.8–21.1 | 0.23 | 9.6** | 8.3** |
| STAI–S | 51.65 | 13.82 | 47.7–55.6 | 46.02 | 14.55 | 41.5–51 | 47.49 | 11.42 | 43.4–51.5 | 46.85 | 13.88 | 42–51.8 | 0.38 | 5.59* | 3.54 |
| STAI–T | 56.53 | 11.79 | 53.1–59.9 | 52.9 | 13.45 | 49–56.8 | 55 | 9.58 | 51.6–58.4 | 54.56 | 11.31 | 50.6–58.5 | 0.00 | 6.17* | 3.8 |
Given the attrition rate, an intention-to-treat analysis was carried out (Table 3). This used scores from the introductory talks for non-attenders in the experimental and control groups at the 3-month stage, assuming no change for these individuals. The results from this analysis also showed significantly superior outcomes on the BDI, GHQ-12 and RSES for the experimental group, as indicated by group × time interactions.
Table 3 Scores of experimental and control groups at baseline and at 3-month follow-up using an intention-to-treat analysis
| Measure | Experimental group (n=60) | Control group (n=60) | Two-way ANOVA (F values) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline score | Follow-up score | Baseline score | Follow-up score | Group | Time | Group × time | |||||||||
| Mean | s.d. | 95% CI | Mean | s.d. | 95% CI | Mean | s.d. | 95% CI | Mean | s.d. | 95% CI | ||||
| BDI | 20.67 | 10.93 | 18–23.4 | 14.81 | 10.4 | 12.2–17.4 | 19.3 | 10.1 | 16.6–22 | 18.4 | 10 | 15.8–21 | 0.39 | 25.1**** | 13.5**** |
| GHQ–12 | 6.2 | 4.16 | 5.2–7.3 | 3.9 | 3.92 | 2.9–4.9 | 6.56 | 4.04 | 5.5–7.6 | 5.74 | 4.12 | 4.7–6.8 | 2.85 | 18.53*** | 4.16* |
| RSES | 16.93 | 8.42 | 14.8–19.1 | 19.73 | 8.58 | 17.6–21.9 | 17.42 | 8.23 | 15.3–19.6 | 17.53 | 8.42 | 15.3–19.7 | 0.34 | 9.25** | 8.0** |
| STAI–S | 48.82 | 13.84 | 47.4–52.2 | 45.07 | 13.81 | 41.5–48.6 | 48.68 | 12.57 | 45.3–52.1 | 48.27 | 14.11 | 44.7–51.8 | 0.44 | 5.53* | 3.54 |
| STAI–T | 55.28 | 11.9 | 52.3–58.2 | 52.87 | 12.9 | 49.7–56.1 | 56 | 11.1 | 53–58.9 | 55.67 | 12.1 | 52.5–58.9 | 0.67 | 6.08* | 3.8 |
DISCUSSION
The large-scale self-confidence workshops appeared to be acceptable to a broad range of the general public, attracting significant numbers, many of whom had not consulted primary care services, and to produce significant improvements over a 3-month period.
Methodological considerations
This is a small preliminary study and is underpowered. In addition, attrition rates were higher than desirable. Much of the attrition occurred between the introductory talks and the workshops, with 27% of the experimental group and 35% of the control group not attending. Although the 3-month wait could explain the attrition rate in the control group, it is not clear why over a quarter of the experimental group said they would like to attend a workshop but did not do so. This issue is being currently investigated in a separate study. However, no difference was found between the baseline scores of those who did not attend and those who did. Intention-to-treat analyses also supported the effectiveness findings.
Effectiveness
The self-confidence workshops led to statistically significant reductions in depression and distress as well as improvements in self-esteem. Although the controlled effect size on the BDI score was small at 0.28 and the clinical significance quite modest, this was in part at least likely to be due to the broad range of scores of the workshop participants. When those with initial BDI scores of less than 14 were excluded, the controlled effect size increased to 0.46. The slightly lower, albeit not significantly different, initial scores of the control group participants who were followed up might also have contributed to this result. Further developments of the workshop programme can be expected to improve its effectiveness.
Recruitment to workshops
These workshops appeared to support the prediction that the change of title from ‘Depression’ to ‘Self-confidence’ would help reach the rather elusive group of people with depression who do not seek medical help. Of the people who attended the introductory talks for whom we had information about previous consultation, 39% had never previously consulted about their depressive problems but nevertheless referred themselves to these workshops and the majority of them (70%) scored above 10 on the BDI. The other 30% had not consulted their general practitioner, scored below this threshold but none the less wished to self-refer, perhaps because they had experienced previously unresolved anxiety and/or depressive problems in the past. Finally, over 94% of those who had previously consulted their general practitioner about their depression scored above the threshold but presumably wanted something more by self-referring.
Given the problems of offering effective treatment to people, this is an important finding, as this route might overcome the reluctance to seek help for depression evinced in the general public and therefore help meet this unmet need. The problem of reluctance is common both in the UK (Bebbington et al, Reference Bebbington, Marsden and Brewin1997, Reference Bebbington, Marsden and Brewin1999) and in Europe, where 43% of those diagnosed with depression failed to seek treatment for their problems (Reference Lepine, Gastpar and MendlewiczLepine et al, 1997). A major public education campaign in the UK (Reference Paykel, Hart and PriestPaykel et al, 1998) left people unconvinced, with 62% admitting they would still be reluctant to consult their general practitioner about their depression for fear of embarrassment and 47% for fear of being judged to be unbalanced or neurotic.
Three-quarters of those who self-referred were identified as ‘probable cases’ on the GHQ-12, indicating that those self-referring were not just a group of the ‘worried well’. These workshops also appeared to attract a population reasonably representative of the local community in terms of ethnicity, employment status and, to a large extent, occupational class. These results have also been found in a more detailed analysis (further details available from the authors on request), which further showed that workshop participants generally had significant mental health problems.
Implications
The results support the hypothesis that this brief, large-scale, day-long psychological intervention can lead to statistically significant improvements in depression, although the attrition rates are higher than desirable and the effect size is relatively small. There was also a statistically significant reduction in distress and improvement in self-esteem with a tendency for associated improvements in anxiety. This approach could consequently have the potential to help address the problem of limited capacity for psychological treatments.
A larger, more rigorous randomised controlled trial is required to confirm the preliminary indication of effectiveness and potential cost-effectiveness. If these are confirmed, this large-capacity intervention might well have the potential to help meet the challenge of reducing the prevalence of this important health problem.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Changing the title of the workshops from ‘Depression’ to ‘Self-confidence’ appears to improve take-up rates and attract those who have not consulted their general practitioner about their depression.
-
▪ Self-confidence workshops conducted in a non-clinical setting can reach a group representative of the population in terms of ethnic background and employment status.
-
▪ The group psycho-educational approach appears to lead to significant improvements in depression, distress and self-esteem.
LIMITATIONS
-
▪ This was a small, preliminary study.
-
▪ Attrition rates were higher than desirable, particularly between the introductory talks and the workshops.
-
▪ The clinical significance of the results may be modest, even though the results are statistically significant.
Acknowledgement
We thank Guy's and St Thomas’ Charitable Foundation for funding this study.









eLetters
No eLetters have been published for this article.