Depression ranks among the most significant health problems in older adults but is potentially treatable at all ages. The consequences of both major and minor depression in older adults are severe and include diminished quality of life, functional decline, marked disability, increased service utilisation and high mortality from comorbid medical conditions. To date, few studies have been published on the incidence of depression in the oldest old and none about its course (Reference Meller, Fichter and SchroppelMeller et al, 1996; Reference Haynie, Berg and JohanssonHaynie et al, 2001; Reference Palsson, Ostling and SkoogPalsson et al, 2001). Given the rapidly increasing number of older adults in society, we studied the incidence and course of depression in the oldest old within the Leiden 85-plus Study.
METHOD
Study design
The Leiden 85-plus Study is a population-based prospective study of a large cohort of community-dwelling older adults in Leiden, The Netherlands. Between 1997 and 1999 all members of the 1912-1914 birth cohort living in Leiden were enrolled in the month of their 85th birthday. No a priori selection criteria with respect to health, cognitive functioning or living situation were applied.
Study setting and procedures
The community of Leiden, consisting of 120 000 inhabitants, is a mostly urban area in the western part of The Netherlands with a mixed socio-economic make-up. Demographic characteristics of the participants were representative of the general Dutch population of 85-year-old persons. Upon enrolment, information was given by mail; further contact was made by telephone or a home visit to ask for approval. Participants were then visited at their place of residence by medical staff and research nurses. During the baseline visits, structured face-to-face interviews were conducted, an electrocardiogram was recorded and blood samples were collected. Follow-up interviews were carried out for all eligible participants each year during the study period of 4 years. The medical ethics committee of the Leiden University Medical Centre approved the study.
Depression
Each year we administered the 15-item Geriatric Depression Scale (GDS-15), a questionnaire especially developed as a screening instrument for the presence of depressive symptoms in elderly populations (Reference Sheik and YesavageSheik & Yesavage, 1986). Depression was considered present when the score on the GDS-15 was 5 points or more. This cut-off gives the best sensitivity and specificity for the presence of major depression in the general population (Reference Sheik and YesavageSheik & Yesavage, 1986), in geriatric in-patients (Reference Shah, Psongsathorn and BielawskaShah et al, 1996), in primary care settings (Reference D'Ath, Katona and MullanD'Ath et al, 1994; Reference Lyness, Noel and CoxLyness et al, 1997) and in medical in-patients (Reference Pomeroy, Clark and PhilpPomeroy et al, 2001), and was found to have a good specificity (0.85) in a representative sample of community-dwelling oldest old for the presence of major depression (Reference de Craen, Heeren and Gussekloode Craen et al, 2003). Because the reliability and the validity of the GDS-15 are compromised in older adults with serious cognitive impairment, the GDS-15 was not administered to participants with a Mini-Mental State Examination (MMSE; Reference Folstein, Folstein and McHughFolstein et al, 1975) score of less than 19 points.
Incidence and course
The incidence of depression was studied by following the participants without depression at baseline, defined as having a GDS-15 score of 0-2 points at age 85 years, over a 4-year period. Incident depression was considered to be present when the GDS-15 increased to 5 points or more during the follow-up measurements.
The course of depression was studied by following the participants with depression at baseline, defined as a GDS-15 score of 5 points or more, for 4 years. Remission of depression was defined as returning to a GDS-15 score of 0-2 points at any measurement during follow-up.
Risk factors
Demographic variables
Gender, marital status, living arrangements, loss of a spouse, income and institutionalisation were recorded. The majority of participants had received only compulsory primary school education; a minority had additional education. Therefore the level of education was dichotomised at 6 years. As low income is a putative risk factor (Reference Cole and DendukuriCole & Dendukuri, 2003) the income was dichotomised across state pension only and state pension plus additional income.
Disability in daily functioning
The Groningen Activity Restriction Scale (GARS; Reference Kempen, Miedema and OrmelKempen et al, 1996) was applied to measure disability in daily functioning. Poor daily functioning was defined as a GARS score above 23 points (33rd percentile). Furthermore, the self-rated presence of loneliness was assessed.
Health-related correlates
Information on the use of medication was obtained from the pharmacists' registers. Data on physical diseases were obtained via a structured questionnaire and based on general practitioners' diagnoses, blood samples and the results of the electrocardiogram. These included cardiovascular disease (stroke, myocardial infarction or ischaemia, arterial surgery, intermittent claudication), malignancy, Parkinson's disease, diabetes mellitus, chronic obstructive pulmonary disease, and arthritic disease at baseline or in the past. Diabetes was considered present in the case of a positive medical history, or current use of antidiabetic medication, or a non-fasting glucose concentration of 11.1 mmol/l or higher.
Statistical analysis
First, to make optimal use of the repetitive measurements and to correct for attrition due to mortality and cognitive decline, the cumulative incidence and the cumulative remission rate of depression with the corresponding 95% CI were calculated from life tables. The assumption was made that depression developed or remitted midway during the follow-up period in which the participant passed the GDS-15 cut-off point. Second, relative risks (and 95% CI) of risk factors for the incidence and the remission of depression were calculated in a Cox proportional hazards model, with the assumption that depression developed or remitted midway during the follow-up period in which the participant passed the GDS-15 cut-off point.
RESULTS
Baseline assessments
During the study period 705 inhabitants of Leiden reached 85 years of age and were eligible to participate. Fourteen died before they could be enrolled and 92 refused to participate. At baseline the response rate was 87%, resulting in a sample of 599 participants. There were no significant differences for various socio-demographic characteristics and the presence of depressive symptoms between the 599 participants and the source population (Reference Bootsma-van der Wiel, van Exel and de CraenBootsma-van der Wiel et al, 2002). Of the 599, 500 had MMSE scores of 19 points or more and were included in the present analysis. Of the 500 participants at baseline, 334 (67%) had no significant symptoms of depression, as evidenced by GDS scores of 0-2 points.
Incidence of depression
During follow-up, the mean total GDS-15 score increased significantly from 0.96 (s.d.=0.80) points at baseline to 2.3 (s.d.=2.7) at age 89 years (paired t-test, P<0.001). Table 1 shows the incidence of depression, defined as a GDS-15 score of 5 points or more, in the 334 participants without depression at baseline. During a follow-up of 827 person-years at risk, depression occurred in 56 participants (incidence rate 68 per 1000 person-years, 95% CI 50-85), amounting to an annual risk of 6.8%. Figure 1 illustrates the cumulative incidence of depression from age 85 to age 89 years.
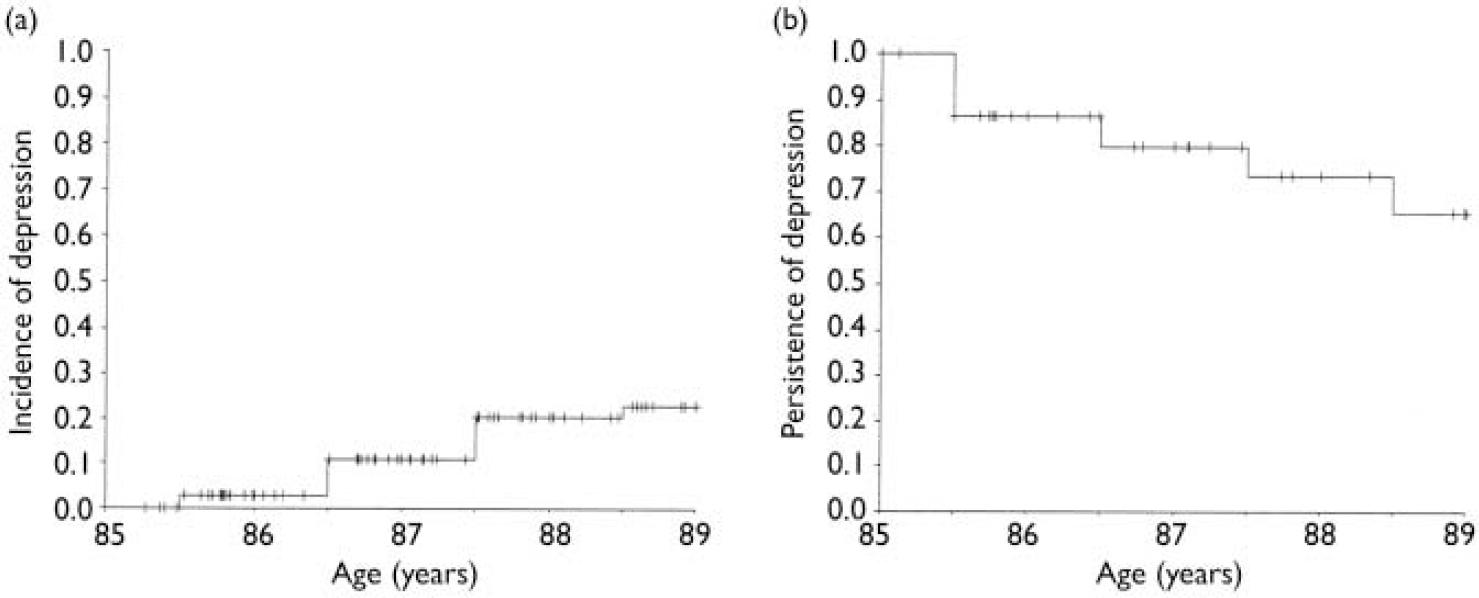
Fig. 1 (a) The cumulative incidence of depression in 334 participants without depression at baseline, defined as a score on the 15-item Geriatric Depression Scale (GDS-15) between 0 and 2 points, from age 85 to 89 years. Incident depression was defined as a GDS-15 score ≥5 points during any of the follow-up measurements.
(b) The cumulative persistence of depression in 77 participants with depression at baseline, from 85 to 89 years. Remission was defined as a GDS-15 score of 0-2 points at any of the follow-up measurements.
Table 1 The incidence of depression 1 during a 4-year follow-up of 334 participants without depression at baseline 2 from age 85 years
| Follow-up year | Participants at start of year (n) | Reasons for attrition | GDS-15 completed | GDS-15 ≥5 points | ||||
|---|---|---|---|---|---|---|---|---|
| Dead | Refusal | Severe cognitive impairement 3 | ||||||
| 1 | 334 | 19 | 24 | 14 | 277 | 8 | ||
| 2 | 269 | 14 | 5 | 9 | 241 | 21 | ||
| 3 | 220 | 17 | 2 | 8 | 193 | 22 | ||
| 4 | 171 | 14 | 8 | 8 | 141 | 5 | ||
GDS-15, 15-item Geriatric Depression Scale.
1. Incident depression was present when the score on the GDS-15 was ≥5 points.
2. Depression was absent when the GDS-15 was 0-2 points.
3. Severe cognitive impairement was present when the Mini-Mental State Examination score was below 19 points.
Risk factors for the incidence of depression
Table 2 shows the impact of various risk factors for the emergence of depression. Neither demographic characteristics nor any of the health-related characteristics contributed to the incidence of depression. Institutionalisation and poor daily functioning were associated with an increased risk of the development of depresssion. The GDS-15 score at baseline was associated with an almost twofold increased risk per point increase. After adjustment for the GDS-15 score at baseline, the increased risks of depression due to institutionalisation (relative risk=2.8, 95% CI 1.3-6.4) and poor daily functioning (relative risk=1.9, 95% CI 1.1-3.4) were sustained.
Table 2 The risk of depression during follow-up in 334 participants without depression at baseline in relation to socio-demographic characteristics, daily functioning and health characteristics
| Characteristic | n(%) | Relative risk (95% CI) 1 | P |
|---|---|---|---|
| Female gender | 209 (63) | 1.1 (0.6-1.9) | NS |
| Low educational level | 195 (58) | 1.0 (0.6-1.7) | NS |
| Low income | 53 (16) | 1.6 (0.8-3.1) | NS |
| Not married 2 | 204 (61) | 0.8 (0.4-1.5) | NS |
| Living alone 2 | 194 (58) | 1.1 (0.7-2.0) | NS |
| Loss of a spouse 2 5 | 56 (17) | 0.9 (0.5-1.7) | NS |
| Presence of loneliness 2 | 29 (9) | 1.3 (0.5-3.3) | NS |
| Institutionalisation 2 | 23 (7) | 3.4 (1.5-7.5) | 0.003 |
| Poor daily functioning 2 3 | 173 (52) | 2.2 (1.3-3.8) | 0.006 |
| Presence of chronic diseases 2 4 | 249 (75) | 1.1 (0.6-2.1) | NS |
| MMSE score 19-23 points 2 | 41 (12) | 0.3 (0.04-2.1) | NS |
| Use of analgesics 2 | 81 (24) | 1.2 (0.7-2.2) | NS |
| Use of benzodiazepines 2 | 56 (17) | 1.1 (0.5-2.2) | NS |
| GDS-15 score at baseline (per point) 2 | - | 1.9 (1.3-2.6) | <0.001 |
GDS-15, 15-item Geriatric Depression Scale; MMSE, Mini-Mental State Examination.
1. Relative risks were estimated with Cox's proportional hazard models.
2. Adjusted for gender, educational level and income.
3. Poor daily functioning defined as a Groningen Activity Restriction Scale score of 24-72 points.
4. Chronic diseases included cardiovascular disease, diabetes mellitus, chronic obstructive pulmonary disease, arthritis, Parkinson's disease and malignancy.
5. Loss of a spouse was introduced in the model as a time-dependent covariate.
Remission of depression
Of the 500 participants at baseline, 77 had GDS scores of 5 points or more, indicating depression (prevalence 15%, 95% CI 12-18%). During the 4-year follow-up we observed a remission in 16 participants, with an annual remission probability of 14% (Fig. 1b). Remission was sustained in 7 of the 16 participants, whereas in 9 participants there was a relapse during follow-up. None of the factors described in Table 2 significantly predicted remission (data not shown).
DISCUSSION
In the present study, we have annually assessed the presence of depression in a large representative sample of community-dwelling oldest old persons. We show that the oldest old are at high risk of developing depression and that, when present, depression is highly persistent. Predictors of depression in the oldest old were institutionalisation and poor daily functioning, but no predictors were identified for remission.
Other studies
In one of the few longitudinal studies of depression in the old-old (79-85 years), Palsson et al (Reference Palsson, Ostling and Skoog2001) reported an incidence of depression according to DSM-III-R criteria (American Psychiatric Association, 1987) of 44 per 1000 person-years, associated with female gender. The lower incidence compared with our estimate of 70 per 1000 person-years is possibly due to the younger age of their participants. An age-associated increase in the incidence of depression is further strengthened by the findings of Meller et al (Reference Meller, Fichter and Schroppel1996), who described a very high incidence of 140 per 1000 person-years in a population of octo- and nonagenarians (85-103 years). Changes in living situation and dementia were the main risk factors in their study, but these did not reach statistical significance. As changes in living situation in this age-group usually mean moving to institutionalised living, this seems to be in line with the finding of institutionalisation as a predictor of depression. The lower incidence of depression reported by Haynie et al (Reference Haynie, Berg and Johansson2001) from the OCTO-Twin study may be explained by their selection of very healthy persons at entry.
Course of depression in the oldest old
In contrast to previous studies on the incidence of depression, no data were available on its course in the oldest old. A strong tendency for chronic depression has been reported in the younger elderly (Reference Beekman, Geerlings and DeegBeekman et al, 2002). Persistence of depression in the younger elderly could be extrapolated to the oldest old.
Possible limitations
An important limitation of our study is that depression was not formally diagnosed. The GDS-15 was originally developed as a screening instrument for depressive illness in older adults, not as a diagnostic procedure. However, given the nature and size of this study, further diagnostic procedures were not feasible. This lack of a second-stage standardised assessment of depression may have resulted in higher incidence and lower remission figures in our study. However, the GDS-15 was found to have a good specificity (0.85) in a representative sample of community-dwelling oldest old for the presence of major depression (Reference de Craen, Heeren and Gussekloode Craen et al, 2003). Moreover, it is becoming increasingly clear that significant depressive symptoms in older adults have as distinct deleterious effects as formally diagnosed depressive disorders (Reference Gallo, Rabins and LyketsosGallo et al, 1997). It could also be questioned whether the GDS-15 is able to detect changes in depressive symptoms over time. Within the Leiden 85-plus Study, we demonstrated that the loss of a partner, which is a major negative life event and an important risk factor for the emergence of depression in older adults, was associated with a significant increase of more than two points on the GDS-15 (Reference Vinkers, Gussekloo and StekVinkers et al, 2004a ). Thus, the chosen GDS-15 criteria for the incidence and remission of depression should enable us to measure a relatively robust change in depressive symptoms over time.
Although the initial response rate in this study was very high, substantial attrition owing to mortality and cognitive decline is an intrinsic part of all prospective studies of depression in the oldest old. In an earlier analysis, we found an almost twofold increased mortality risk for oldest old participants of the Leiden 85-plus Study with depression; this was sustained when corrected for demographic and health-related factors (Reference Stek, Vinkers and GusseklooStek et al, 2005). In the present study, refusal to participate was not related to depression at baseline (Reference Bootsma-van der Wiel, van Exel and de CraenBootsma-van der Wiel et al, 2002), but participants with incident depression might have refused more often at follow-up. Confounding by effects of specific treatment is probably very limited because, as reported before, the use of antidepressants was almost non-existent at baseline (Reference Stek, Gussekloo and BeekmanStek et al, 2004). We did not identify determinants that predicted remission, but as depression is associated with refusal and mortality, the numbers in our study might have been too small to detect these effects.
Role of cognitive functioning and early dementia
Depression and early dementia are closely linked. Earlier we showed that cognitive impairment at baseline predicted an accelerated increase of depressive symptoms in the oldest old, whereas depression at baseline was not related to increased cognitive decline (Reference Vinkers, Gussekloo and StekVinkers et al, 2004b ). Thus, cognitive impairment preceded depression but depression did not herald cognitive decline. Cognitive impairment or early-stage dementia might well play an important role in the high incidence of depression and its persistence in the oldest old, but the underlying mechanisms are still unresolved. Since participants who developed serious cognitive impairment (MMSE <19 points) were excluded from our study, incidence rates for depression may even have been underestimated.
Treatment of depression in the oldest old
Notwithstanding a lack of knowledge about the origins of depression in the oldest old, from a clinical perspective it is very important that depression occurs often in this age-group and has a poor prognosis. Poor daily functioning and institutionalisation are strong predictors of incident depression in the oldest old. In an earlier study of the oldest old (Reference Stek, Gussekloo and BeekmanStek et al, 2004), the recognition of depression by the general practitioner was poor and antidepressive treatment virtually non-existent. Taken together with the results of the present study, it is clear that more active case-finding is warranted, as treatment of depression in the oldest old is as potentially rewarding as in younger people.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Depression occurs frequently and is highly persistent in the oldest old.
-
▪ Poor daily functioning and institutionalisation at baseline predicted depression.
-
▪ More active case-finding and treatment of depression in the oldest old would be potentially rewarding.
LIMITATIONS
-
▪ Depression was not formally diagnosed.
-
▪ Participants with severe cognitive impairment (Mini-Mental State Examination score of less than19) were excluded from the analyses.
-
▪ Substantial attrition due to mortality and cognitive decline is an intrinsic part of all prospective studies of depression in the oldest old.








eLetters
No eLetters have been published for this article.