Although attention-deficit hyperactivity disorder (ADHD) has long been thought to be a disabling and common disorder that occurs only in childhood, more recent research, including prospective longitudinal follow-up studies, suggests that ADHD persists into adulthood in a high proportion of cases. Reference Barkley, Fischer, Smallish and Fletcher1–Reference Weiss, Hechtman, Milroy and Perlman8 Adult ADHD studies indicate a high degree of genetic predisposition, Reference Smalley, McGough, Del'Homme, NewDelman, Gordon and Kim9,Reference Faraone and Doyle10 and reveal structural and functional brain abnormalities Reference Castellanos, Lee, Sharp, Jeffries, Greenstein, Clasen, Blumenthal, James, Ebens, Walter, Zijdenbos, Evans, Giedd and Rapoport11–Reference Schweitzer, Faber, Grafton, Tune, Hoffmann and Kilts14 congruent with neuropsychological data. Reference Schweitzer, Faber, Grafton, Tune, Hoffmann and Kilts14–Reference Seidman, Biederman, Webwe, Hatch and Faraone16 Attention-deficit hyperactivity disorder is a serious risk factor for comorbid psychiatric disorders (antisocial personality disorder, substance misuse and affective disorders), Reference Wilens, Faraone and Biederman17,Reference Biederman, Faraone, Spencer, Wilens, Norman, Lapey, Mick, Lehman and Doyle18 and also shows significant correlation with poor socio-economic outcome and functional impairment (lower level of education, higher level of unemployment, and higher rates of unsuccessful marriages, criminality and road traffic accidents). Reference Barkley, Fischer, Smallish and Fletcher1,Reference Mannuzza, Klein, Bessler, Malloy and LaPadula7,Reference Weiss, Hechtman, Milroy and Perlman8,Reference Biederman, Faraone, Spencer, Wilens, Norman, Lapey, Mick, Lehman and Doyle18–Reference Biederman, Faraone, Spencer, Mick, Monuteaux and Aleardi23
In spite of the growing literature dealing with adult ADHD, relatively little is known about the prevalence of the disorder among adults and its correlates. To our knowledge no meta-analysis of the epidemiological data on adult ADHD has been published. The aim of our study was to estimate the prevalence of ADHD in adulthood using a meta-regression approach and to identify demographic factors that might influence the prevalence of ADHD in a given population.
Method
Study selection
We searched MEDLINE, PsycLit and EMBASE for publications dealing with the epidemiology of adult ADHD. Only publications in English were considered. As a first step, we created four databases with the keywords ADULT, ADHD, EPIDEMIOLOGY and PREVALENCE respectively. Second, we connected the ADULT and ADHD databases with a logical ‘and’ operation, generating a new database containing only those publications that were part of both ADULT and ADHD databases in the first step. The other two databases (EPIDEMIOLOGY and PREVALENCE) were connected with the ‘or’ operation, creating a new database including all publications that were originally in the EPIDEMIOLOGY and PREVALENCE databases. During the final step, the two new databases were connected with the ‘and’ operation. In addition to this search procedure, we used the reference lists of the identified publications to find further relevant articles. After excluding follow-up and family studies–which do not provide prevalence data for adult ADHD–and studies that dealt with the prevalence of ADHD in special groups (people with panic or bipolar disorder, drug addiction or obesity, or people in prison), 12 population-based studies remained:
-
(a) one study estimated the cumulative incidence of ADHD at the age of 19 years based on retrospective analysis; Reference Barbaresi, Katusic, Colligan, Weaver, Pankratz, Mrazek and Jacobsen24
-
(b) one study estimated the prevalence of adult ADHD among licensed drivers; Reference Murphy and Barkley25
-
(c) three studies estimated the prevalence of ADHD among university students; Reference Weyandt, Linterman and Rice26–Reference Heiligenstein, Conyers, Berns and Smith28
-
(d) one study estimated the prevalence of ADHD among a non-clinical sample from an out-patient psychiatric service; Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29
-
(e) six studies provided a community-based estimate: oppositional defiant disorder only and ADHD only v. oppositional defiant disorder + ADHD in clinic and community adult samples; Reference Gadow, Sprafkin, Schneider, Nolan and Schwartz30 a cross-national survey; Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31 the National Comorbidity Survey Replication; Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32 the Mexican National Comorbidity Survey; Reference Medina-Mora, Borges, Lara, Benjet, Blanco, Fleiz, Villatoro, Rojas and Zambrano33 a telephone survey; Reference Faraone and Biederman34 and the Nijmegen Health Area Study 2. Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19
For our meta-regression analyses six studies were omitted. Three of these studies (Kessler et al, Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32 Medina-Mora et al Reference Medina-Mora, Borges, Lara, Benjet, Blanco, Fleiz, Villatoro, Rojas and Zambrano33 and Fayyad et al Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31 ) were not included because they did not provide raw data for the prevalence and demographic variables necessary for the computations. The study by Barbaresi et al Reference Barbaresi, Katusic, Colligan, Weaver, Pankratz, Mrazek and Jacobsen24 was not included because it dealt only with the cumulative incidence of ADHD between the ages of 5 and 19 years and accordingly provided information about ADHD in adolescents rather than in adults. The study by Weyandt et al Reference Weyandt, Linterman and Rice26 was not included because it measured only the prevalence of attention-deficit symptoms and not the prevalence of adult ADHD. Finally, we omitted the study by Gadow et al Reference Gadow, Sprafkin, Schneider, Nolan and Schwartz30 because these authors did not use DSM–IV 35 criteria for the diagnosis of adult ADHD. The modified diagnostic criteria used by Gadow et al did not include age at onset or functional impairment criteria, and applied a threshold of five rather than six symptoms. Reference Gadow, Sprafkin, Schneider, Nolan and Schwartz30 Lowering the diagnostic threshold concerning symptom counts has a dramatic effect on prevalence estimates; inclusion of data based on a lower symptoms threshold would therefore have introduced substantial heterogeneity in the meta-analysis.
Variables
For the purpose of the meta-analysis we extracted the following domains or variables from the articles that were finally included:
-
(a) data describing the study–date of publication, country, number of arms;
-
(b) data describing the target population–sample size, mean age, age range, standard deviation for age range, gender composition (proportion of males in the sample);
-
(c) diagnostic tools for adult ADHD–self-report, structured interview;
-
(d) results–prevalence rate according to DSM–IV criteria (total and subtypes if provided), prevalence rate according to alternative criteria, if available (total and subtypes, if given).
Statistical analysis
A mixed-effect (with fixed and random effects) meta-regression–a meta-analytic technique of multivariate linear regression across studies–was applied to estimate the prevalence of ADHD across various study samples and in order to evaluate the impact of potential demographic variables of interest including age and gender on the prevalence estimates. The meta-regression analysis that we adopted in this investigation was based on van Houwelingen et al's general linear mixed-model technique based on the approximate likelihood approach. Reference van Houwelingen, Arends and Stijnen36 In particular, the log-odds of the observed prevalence in each study were regressed using intercept and basic study-level demographic covariates that included average age and gender composition from each of the individual studies. Interaction between the two covariates (age, gender composition) was also included in the model. In addition, a random-effect intercept term representing systematic between-study variation (heterogeneity) was also incorporated in the meta-regression model. A common weighted prevalence estimate for ADHD was calculated as a DerSimonian & Laird estimator, based on the random effects component of the mixed model that incorporated both fixed and random effects. Reference DerSimonian and Laird37
Results
Study design
In all the articles included in the analysis we found that although the sample sizes were large (typically several hundreds of participants), the authors collected samples of convenience, which do not assure representativeness. Accordingly, the raw estimates of prevalence from these studies cannot be extended to the general population. We note that in the study by Faraone & Biederman, Reference Faraone and Biederman34 raw prevalence estimates were weighted by US census data (based on age, ethnicity, education, geographic region and number of telephone lines within the household) in order to derive prevalence estimates generalisable for the population; however, the final derived prevalence estimates remain questionable in light of the high refusal rate (approximately 80%) in the target population that was used to derive the prevalence estimates in the sampling phase of the study. In the study by DuPaul et al,in addition to the problem with representativeness, there were remarkable differences across the three subsamples in terms of the number, gender and age range of the participants (Tables 1 and 2). Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27
Table 1 Demographic data of samples included in the meta-analysis

| Age, years | |||||
|---|---|---|---|---|---|
| Study | Sample size, n | Mean (s.d.) | Range | Gender proportions Male/female, % | |
| Murphy & Barkley Reference Murphy and Barkley25 | 720 | 35 (13.2) | 17–84 | 60/40 | |
| Heiligenstein et al Reference Heiligenstein, Conyers, Berns and Smith28 | 448 | 20.6 (4) | 17–46 | 56/44 | |
| Du Paul et al Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27, a | 1209 | ||||
| Italy | 197 | 21.6 (3) b | 18–35 | 14/86 b | |
| New Zealand | 213 | 19.4 (4) | 17–51 | 17/83 | |
| USA | 799 | 21.3 (4.9) | 17–49 | 51/49 | |
| Kooij et al Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19 | 1815 | 44.9 c | 18–75 | 45/55 | |
| Faraone & Biederman Reference Faraone and Biederman34 | 966 | 35.9 d | 48/52 | ||
| Almeida Montes et al Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29 | 149 | 28.5 | 32.9/67.1 | ||
a. Data available separately by subsample (country) in the original publication
Table 2 Descriptive data for studies included in the meta-analysis

| Design | Diagnostic procedure | |
|---|---|---|
| Murphy & Barkley Reference Murphy and Barkley25 | One-stage sampling | DSM–IV symptom list |
| Community-based study | Self-report | |
| Non-representative, sample of convenience | ||
| Heiligenstein et al Reference Heiligenstein, Conyers, Berns and Smith28 | One-stage sampling | DSM–IV symptom list |
| College students | Self-report | |
| Non-representative, sample of convenience | No data from childhood | |
| DuPaul et al Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27 | One-stage sampling | DSM–IV symptom list |
| Three study arms | Self-report | |
| University students | No data from childhood | |
| Non-representative, sample of convenience | ||
| Kooij et al Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19 | One-stage sampling | DSM–IV |
| Community-based study in general practices | Modified Dutch version of DSM–IV ADHD | |
| Non-representative, probability sample | Rating Scale | |
| Self-report and structured interview | ||
| Faraone & Biederman Reference Faraone and Biederman34 | One-stage sampling | DSM–IV symptom list |
| Community-based telephone survey | Self-report | |
| Non-representative, probability sample | ||
| Almeida Montes et al Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29 | One-stage sampling | DSM–IV |
| Non-clinical population from a psychiatric out-patient service | MINI | |
| Non-representative, sample of convenience | Structured interview |
ADHD, attention-deficit hyperactivity disorder; MINI, Mini International Neuropsychiatry Interview
b. Our calculation from the given data (number of females and males in all groups)
c. Our calculation from the given proportion of age range groups and numbers of participants
d. Derived from US census data referred to in the original article
Age
In most of the studies, the sample's mean age was low compared with the mean age of a typical adult population. Specifically, although the mean ages were 19.4–44.9 years for all samples in the analysis (the mean age, weighted by the number of participants in each study, was 34 years), for the majority of samples the mean age ranged between 19.4 and 28.5 years. Only one study had a mean age of 44.9 years, Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19 whereas two studies had a mean age of around 35 years. Reference Murphy and Barkley25,Reference Faraone and Biederman34 (Of these two studies, Faraone & Biederman provided estimates for mean age based on weighting using the US census data; Reference Faraone and Biederman34 Table 1).
Gender
With the exception of one study sample (the USA arm of the study by DuPaul et al), Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27 the gender proportions were neither balanced nor representative of the target population. There were extreme differences in the male: female ratio across the groups in the study by DuPaul et al, Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27 with a substantial departure from the population gender distribution in two arms of this study, possibly as a result of the above-mentioned convenience sampling (Table 1).
Diagnosis
The studies included in our meta-analysis applied different methodology and design with regard to sampling and diagnosing adults with ADHD (Table 2). All studies employed DSM–IV diagnostic criteria, even though all–except for Faraone & Biederman Reference Faraone and Biederman34 and Almeida Montes et al Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29 –questioned the validity of DSM–IV criteria for ADHD when applied to adults. 35 In terms of association between symptoms that underlie the DSM–IV diagnosis of adult ADHD and functional impairment (used as an external validator of the disorder), Kooij et al found the strongest association from four symptoms being present (as opposed to the threshold of six symptoms according to the DSM–IV diagnostic system). Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19 DuPaul et al Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27 and Heiligenstein et al Reference Heiligenstein, Conyers, Berns and Smith28 applied alternative diagnostic criteria with a lower threshold, besides the original DSM–IV criteria. Although Murphy & Barkley used only DSM–IV diagnostic criteria in their study, they suggested the possibility of modifying these criteria for adult ADHD in future. Reference Murphy and Barkley25 Faraone & Biederman considered two types of diagnoses for adult ADHD: a ‘broad’ diagnosis for screening purposes, which followed the DSM–IV criteria but was more inclusive concerning symptom severity; and a ‘narrow’ diagnosis based solely on DSM–IV criteria. Reference Faraone and Biederman34
Estimated prevalence and correlates of adult ADHD
Mixed-effect meta-regression analysis was applied to estimate the prevalence across samples and to investigate prevalence as a function of gender composition and mean age in the respective samples. Results of the meta-regression analysis indicated that the pooled prevalence of ADHD across samples was 2.5% (95% CI 2.1–3.1; t=42.3, P<0.0001) (Fig. 1).
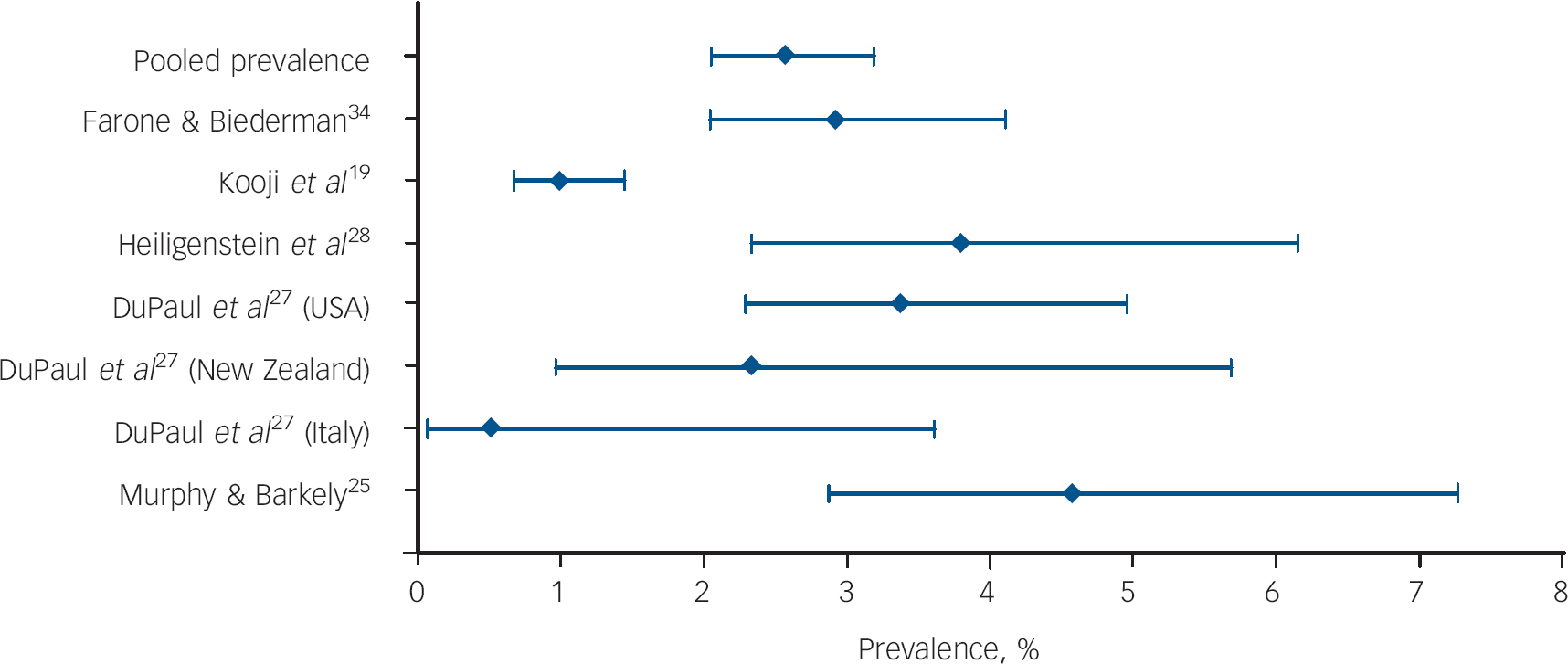
Fig. 1 Prevalence estimates and 95% confidence intervals of adult attention-deficit hyperactivity disorder in individual investigations and pooled prevalence estimated across studies using meta-regression analysis.
Adopting the likelihood approach as recommended by Hardy & Thompson Reference van Houwelingen, Arends and Stijnen36 and van Houwelingen, Reference Hardy and Thompson38 heterogeneity among studies included in the meta-analysis was tested by the likelihood ratio statistic, by comparing the maximum log-likelihood (LL) of the random-effect model with that of the fixed-effect model. Our results showed that the random and fixed-effects models yielded maximum LL values of–9.9 and–42.5 respectively. This indicates a statistically significant heterogeneity across studies (χ2=65.2, d.f.=1, P<0.0001), which (as shown by subsequent analyses) was due, at least in part, to the principal demographic variables that we examined in our study. In particular, our results showed that the prevalence of ADHD was significantly related to the gender composition in the sample (t=4.34, P=0.012, standardised beta for log-odds of observed prevalence 15.19 × 10–2) and to the mean age (t=3.03, P=0.039, standardised beta for log-odds of observed prevalence 20.98 × 10–2). Furthermore, the interaction between the two covariates also reached statistical significance (t=–3.42, P=0.027, standardised beta for log-odds of observed prevalence 0.50 × 10–2). The association between the proportion of participants with ADHD and gender composition and mean age is shown in Fig. 2. Owing to the statistically significant interaction reported above, for illustrative purposes the association of prevalence with gender composition is displayed at various ages (20, 30 and 40 years; Fig. 2(a)); for younger age groups the prevalence increases, whereas for the older age group prevalence decreases with higher proportion of males in the sample. Analogously, for illustrative purposes the association of prevalence with mean age was broken down by male percentage of the sample (a third, a half, two-thirds; Fig. 2(b)); the prevalence decreases with age when men are represented at 50% or more in the sample, but increases with age when women are predominantly represented in the sample (male proportion, 33.3%).
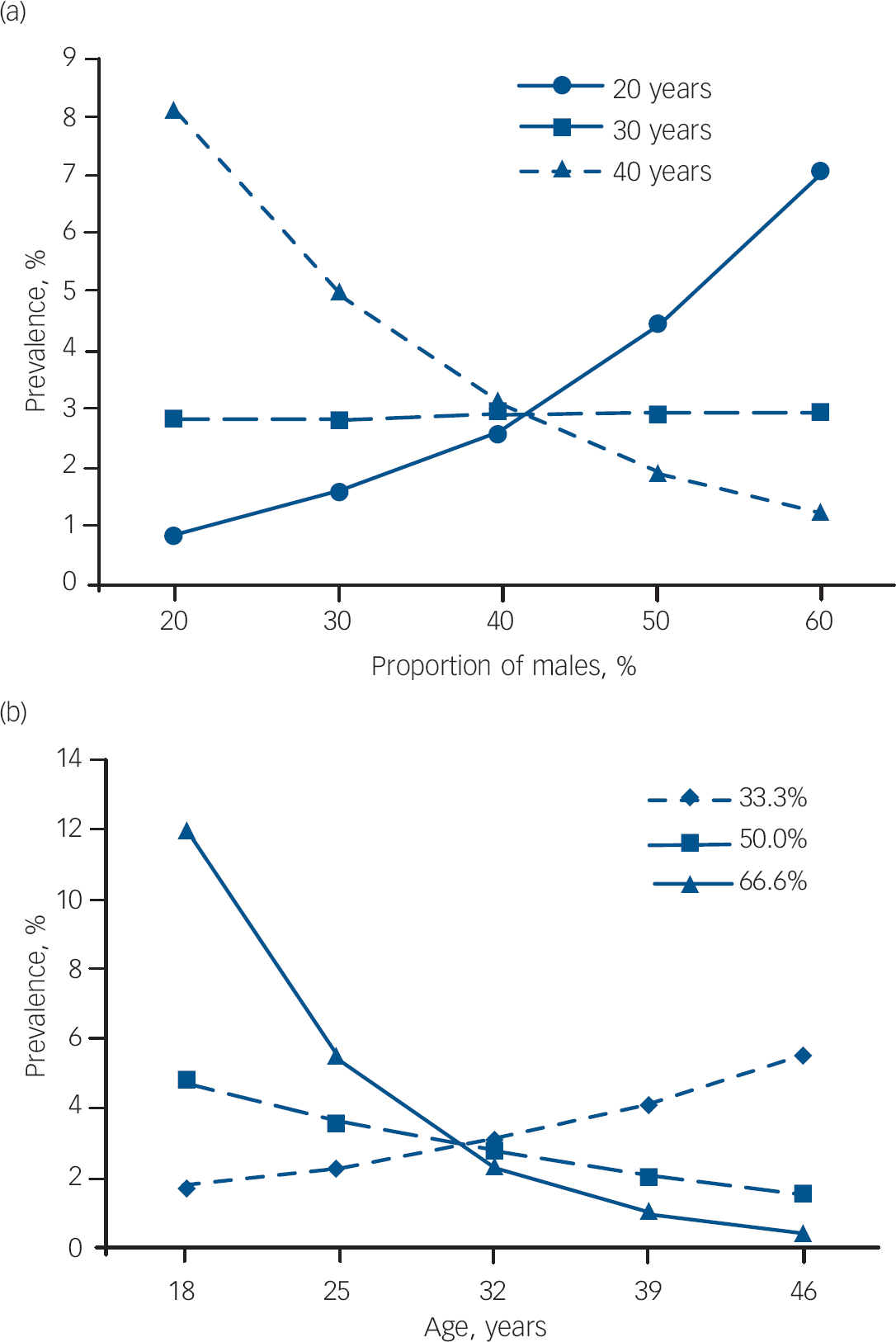
Fig. 2 Relationship between gender composition (% male) and prevalence (%) of adult attention-deficit hyperactivity disorder (ADHD). Meta-regression analysis indicated that gender and mean age, interacting with each other, were statistically significantly related to the prevalence of ADHD in the sample. (a) Relationship between gender composition and prevalence at ages 20, 30 and 40 years. (b) Relationship between age and prevalence as a function of gender composition (a third, a half, two-thirds males).
We note that the above results are based on prevalence data that relied on DSM–IV diagnostic criteria. Individual studies included in our meta-analysis used other diagnostic criteria as well, but these alternative criteria varied between studies, precluding a meaningful pooling of the results. Indeed, as Table 3 shows, these alternative thresholds lead to substantial variation in the results (prevalence between 2.5% and 42.3%), reflecting the heterogeneity of the alternative diagnostic approaches in the individual studies.
Table 3 Results of the studies included in the meta-analysis

| Prevalence defined by DSM–IV criteria, % | Prevalence defined by criteria other than DSM–IV, % | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total a | I a | HI | Comb. | Total a | I a | HI | Comb. | |||||||
| Murphy & Barkley Reference Murphy and Barkley25 | 4.7 | 1.3 | 2.5 | 0.9 | No data available | |||||||||
| Heiligenstein et al Reference Heiligenstein, Conyers, Berns and Smith28 | 4 | 2.24 b | 0.88 | 0.88 | 11 | 3.74 b | 3.96 | 3.30 | ||||||
| Reduced number of symptoms required (4) | ||||||||||||||
| DuPaul et al Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27 | ||||||||||||||
| Italy | 1.01 | 0.51 b | 0.51 | 0 | 42.31 | 8.82 b | 23.42 | 98.68 | ||||||
| New Zealand | 2.81 | 0.47 b | 2.34 | 0 | 36.06 | 9.50 b | 17.08 | 9.48 | ||||||
| USA | 3.39 | 0.75 b | 2.15 | 0.5 | 26.91 | 4.97 b | 13.90 | 7.15 | ||||||
| Reduced number of symptoms required (3) | ||||||||||||||
| Kooij et al Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19 | 1 | 0.2 | 0.5 | 0.3 | 2.5 | 0.3 | 1.2 | 1.0 | ||||||
| Reduced number of symptoms required (4) | ||||||||||||||
| Faraone & Biederman Reference Faraone and Biederman34 | 2.9 | 0.7 | 1.1 | 1.1 | 16.4 | 5.8 | 3.7 | 6.9 | ||||||
| ‘Broad’ ADHD c | ||||||||||||||
| Almeida Montes et al Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29 | 5.37 | No data available | ||||||||||||
ADHD, attention-deficit hyperactivity disorder; Comb., combined subtype; HI, hyperactive–impulsive subtype; I, inattentive subtype
a. Total: all subtypes of ADHD pooled (inattentive subtype, hyperactive–impulsive subtype, combined subtype)
b. Our calculation from data given in the original article
c. Referred as screening diagnosis in the original article
Discussion
In general, epidemiological data about adult ADHD have been collected from three different sources: family studies, follow-up studies and population-based studies. In family studies, parents of children who did not have ADHD–who had taken part in case–control ADHD studies as the control group–were examined for adult ADHD. The results of these studies cannot be generalised since they used a strongly selected sample, excluding a genetically predisposed group–parents of children with ADHD. Reference Faraone and Biederman34
Follow-up studies are long-term prospective studies designed to determine the persistence of ADHD among adolescents and adults by following an index ADHD group of school-aged children and a matched control group. Follow-up studies show that ADHD persists in 4–66% of the cases into adulthood. Reference Barkley, Fischer, Smallish and Fletcher1–Reference Weiss, Hechtman, Milroy and Perlman8 Such variability in the persistence of the disorder into adulthood can be explained–at least in part–by methodological differences such as small sample sizes; non-representative, predominantly clinical samples; different diagnostic criteria among and across studies; and changing the source of information during the follow-up from parent report to self-report only. These methodological differences imply that follow-up studies are difficult to compare and the results of those studies can neither be generalised nor used for estimating prevalence of ADHD in adulthood.
Population-based studies estimated prevalence rates of adult ADHD at 1–7.3% applying DSM–IV criteria. Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19,Reference Barbaresi, Katusic, Colligan, Weaver, Pankratz, Mrazek and Jacobsen24,Reference Murphy and Barkley25,Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27–Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29,Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31–35 Most of these studies were designed for direct estimation of the prevalence of adult ADHD in a target population such as a community, university students, prisoners or a special population of patients. These studies typically used a large sample and therefore were usually appropriate for estimating prevalence with sufficient precision. However, they did not assure representativeness, since they were based on a sample of convenience. In general, the mean age of the participants was low compared with a typical adult population, and there were several studies in which the gender proportion of the sample was significantly unbalanced. In addition, the diagnostic tools and the approach for the identification of cases usually varied from study to study.
Gadow et al provided estimates of the prevalence of adult ADHD using a large, representative sample of the general population. Reference Gadow, Sprafkin, Schneider, Nolan and Schwartz30 Nevertheless, because these authors applied only modified diagnostic criteria, their prevalence data are difficult to compare with the prevalence estimates from other studies that relied on the original DSM–IV classification. Two studies, being parts of large-scale epidemiological surveys–the National Comorbidity Survey Reference Kessler and Merikangas39 and the World Health Organization (WHO) World Mental Health Surveys Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureye, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennel, Zaslavsky, Üstün and Chatterji40 –did not provide crude estimates for the prevalence of adult ADHD in their sample; they used indirect estimation in order to assess the prevalence of adult ADHD in the general population. The first of these studies (Kessler et al Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32 ) examined an US sample, whereas the second (Fayyad et al Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31 ) estimated cross-national prevalence in ten countries. We note that despite these two studies applying the same general approach, the first estimated prevalence at 4.4%, Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32 whereas the second estimated the prevalence in the US sample at 5.2%. Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31 Based on the authors' comments, this discrepancy is attributable to the fact that certain predictors for the prevalence estimation that were used in the first (USA only) study were not available in the second (multinational) study. In the second study, the prevalence estimates of adult ADHD across samples showed a substantial variation: they were between 1.2% and 7.3%, with an estimated general cross-national prevalence of 3.4%. Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31 In both studies, prevalence estimates were based on multiple imputation using a combination of directly interviewed cases and multiply imputed cases from the remainder of the sample. In all cases (directly interviewed and multiply imputed) in both samples the individuals were aged 18–44 years; prevalence estimates for higher age ranges were based on weighting data. Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31,Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32 The aforementioned indirect estimations (applied in both studies) of the prevalence of adult ADHD in the general population hinge on prediction equations that were obtained in a relatively small sample (n=154). It is not clear how reliably these equations can predict the occurrence of ADHD, and what the exact predictors are. With regard to the multinational study, it must be noted that the prediction equation of the US sample was extrapolated to other countries, a potential limitation pointed out by the authors. A third study, conducted as part of the WHO survey, estimated the 12-month prevalence of ADHD in Mexico; Reference Medina-Mora, Borges, Lara, Benjet, Blanco, Fleiz, Villatoro, Rojas and Zambrano33 however, like the parent study it did not provide a crude prevalence estimate for the targeted sample and therefore was not included in our meta-analysis.
In summary, published estimates of the prevalence of adult ADHD vary greatly. Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19,Reference Murphy and Barkley25,Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27–Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29,Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31–Reference Faraone and Biederman34 After reviewing the pertinent publications, we attributed this variability to methodological and diagnostic differences between the studies. In addition, only self-reports were used as a source of information and in some studies there was a lack of information about the relevant childhood symptoms that would be necessary for the proper diagnosis of adult ADHD. Reference Weyandt, Linterman and Rice26–Reference Heiligenstein, Conyers, Berns and Smith28
Correlation of prevalence with gender and age
Our finding of a pooled prevalence rate for adult ADHD of 2.5% (95% CI 2.1–3.1) seems to be conservative in the context of the research discussed above. Our pooled prevalence estimates were derived from studies that provided data for crude prevalence based on strict DSM–IV criteria for diagnosing ADHD. In two of these studies, however, indirect estimates were derived by assessing ADHD symptoms in childhood and asking only a single question about the persistence of problems with ADHD into adulthood. Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31,Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32
Polanczyk et al recently estimated the worldwide prevalence of ADHD in a meta-regression analysis of 102 articles regarding child and adolescent ADHD. Reference Polanczyk, De Lima, Horta, Biederman and Rohde41 Although the pooled prevalence of ADHD in children and adolescents according to these authors was 5.29%, they also reported that the prevalence in adolescents was around 3%. Reference Polanczyk, De Lima, Horta, Biederman and Rohde41 This estimate is consistent with our pooled prevalence data, especially in light of the finding about the relationship between age and prevalence of ADHD.
A growing number of studies indicate that biased samples might underlie extreme gender effects on the prevalence of ADHD in clinically referred paediatric study samples. Specifically, some of these studies suggest that a weaker association with conduct disorder and disruptive behaviour in girls compared with boys might result in lower numbers of female referrals. Reference Biederman, Kwon, Aleardi, Chouinard, Marino, Cole, Mick and Faraone42–Reference Gaub and Carlson44 In contrast to the clinical samples, in which male: female ratios as high as 10: 1 have been observed, Reference Biederman, Mick, Faraone, Braaten, Doyle, Wilens, Spencer, Frazier and Johnson45,Reference Arnold46 community samples showed a less extreme gender ratio (male: female risk 3: 1) in the prevalence of ADHD in childhood. Reference Biederman, Faraone, Monuteaux, Bober and Cadogen43,Reference Gaub and Carlson44 Compared with paediatric and adolescent studies, adult ADHD studies have generally shown a more balanced distribution of prevalence in men and women. This may be attributable to the fact that whereas childhood referrals are usually initiated by parents or teachers, in adulthood self-referrals are common. The observation that women with ADHD have more internalising problems than men, which leads to a higher rate of self-referrals in adulthood, Reference Gershon47 may underlie the more balanced gender ratio in adult samples.
In the studies that were included in our analysis, samples were community-based and the authors found heterogeneous gender ratios but no significant gender effect on prevalence in their samples when applying DSM–IV diagnostic criteria. Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19,Reference Murphy and Barkley25,Reference DuPaul, Schaughency, Weyandt, Tripp, Kiesner, Ota and Stanish27–Reference Almeida Montes, Hernandez Garcia and Ricardo-Garcell29,Reference Faraone and Biederman34 In two studies that were not included in our meta-analysis owing to the lack of crude prevalence data, Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31,Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32 the authors found modest gender effects on prevalence, with a significantly higher proportion of men in their ADHD group. In spite of the findings of the studied articles that supported no significant gender effect on prevalence, using the raw data of the individual studies we identified gender as another factor that has an impact on the prevalence of adult ADHD. In this case – as in the case of effect of age – we presume that methodological differences and questions concerning sample selection and case identification underlie the absence of or modest appearance of gender effects in community-based samples.
Our findings indicate that the prevalence of adult ADHD has a significant negative association with age, although this association is moderated by the gender composition of the sample. The explanation and the potential practical use of this finding are complex. Specifically, available literature and clinical experience indicate a modulation of the presentation of symptoms of ADHD by adulthood. Reference Wender, Wolf and Wasserstein48–Reference Biederman, Mick and Faraone50 Conceptualisation of ADHD as a developmental disorder entails that, although the disabling feature of the disorder remains, both the quality and the severity of symptoms may change over time. Thus, applying the diagnostic criteria created for children may not be appropriate in adulthood. The developmental nature of the disorder also means that although new cases do not emerge in adulthood, there might be a certain number of children who ‘outgrow’ the disorder. This concept predicts reduced prevalence in adulthood because of the nature of the disorder. In view of our finding of a significant age–gender interaction, this concept might be mainly true for male ADHD cases with more hyperactive symptoms and linked disruptive behavioural problems than female ADHD cases in general.
Several studies reported that symptoms of ADHD declined with age. Reference Murphy and Barkley25,Reference Heiligenstein, Conyers, Berns and Smith28,Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31,Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Üstün, Walters and Zaslavsky32,Reference Faraone and Biederman34,Reference Hill and Schroener51 At the same time, functional impairment and low socio-economic outcome can be detected even with a reduced number of symptoms Reference Kooij, Buitelaar, van den Oord, Furer, Rijnders and Hodiamont19,Reference Biederman, Faraone, Spencer, Mick, Monuteaux and Aleardi23,Reference Fayyad, De Graaf, Kessler, Alonso, Angermeyer, Demyttenaere, De Girolamo, Haro, Karam, Lara, Lepine, Ormel, Posada-Villa, Zaslavsky and Jin31,Reference Polanczyk, De Lima, Horta, Biederman and Rohde41,Reference Wender, Wolf and Wasserstein48 These observations lead us to another possible conclusion, that some children with ADHD do not outgrow the disorder but ‘outgrow the diagnostic criteria’, Reference Barkley, Fischer, Smallish and Fletcher1 meaning that reduced prevalence among adults results from an underestimation of the true prevalence of adult ADHD. Our finding that prevalence increases with age when women are predominantly represented in the sample might relate to the previously mentioned possibility of ‘pseudo-new’ cases of ADHD, when women with this disorder who were not referred for treatment in childhood owing to the absence of disruptive behavioural problems refer themselves in adulthood because of emerging comorbid psychiatric disease.
Two other factors concerning the diagnosis of adult ADHD should be mentioned, since either of them may result in underestimation of the prevalence of the disorder. First, based on the finding of the Milwaukee study, Reference Barkley, Fischer, Smallish and Fletcher1 – relevant also to clinical experience – it seems that the source of information might have a great impact on diagnosing ADHD: the persistence of ADHD was five to nine times higher when based on parent's report than when based on self-report, and parent's reports also showed higher potential to predict functional impairment than did self-report. Reference Barkley, Fischer, Smallish and Fletcher1 The second factor is the problem of symptom recall. Several authors pointed out that collecting data with retrospective self-report would underestimate the prevalence of adult ADHD, since adults do not remember their childhood symptoms properly. Empirical findings are inconsistent concerning this issue. Reference Barkley, Fischer, Smallish and Fletcher1,Reference Mannuzza, Klein, Klein, Bessler and Shrout52–Reference Holmshaw and Simonoff60 In the Milwaukee follow-up study, at the adult follow-up only 47% of the participants recalled having ADHD in childhood from the original ADHD index group. Reference Barkley, Fischer, Smallish and Fletcher1 Their self-report showed only 20% concordance with their parents' report concerning their childhood symptoms. Reference Barkley, Fischer, Smallish and Fletcher1 Manuzza et al on the other hand, in the results of the New York follow-up study, reported good symptom recall (the sensitivity of retrospective diagnosis of ADHD was 0.78 and the specificity was 0.89) based on self-reports in the index group at the adult follow-up. Reference Mannuzza, Klein, Klein, Bessler and Shrout52 These authors noted that this might result from the fact that participants in the index group were from a clinically referred sample. Moreover, they suggested that adults who were not hospitalised in their childhood might have had poorer symptom recall. Reference Mannuzza, Klein, Klein, Bessler and Shrout52 The fact that in the New York study there was a high rate of false positive cases in the control group, according to Manuzza et al, Reference Mannuzza, Klein, Klein, Bessler and Shrout52 raises the possibility of problematic symptom recall among people who do not have ADHD.
In summary, we think that our finding is consistent with the suggestion that the prevalence of ADHD declines with age; however, the background of this phenomenon remains unclear and a caveat is needed in this regard. Specifically, the validity of DSM–IV diagnostic criteria for diagnosing adult ADHD is an important issue, emerging both from the interpretation of our findings and also from the relevant literature. It seems that diagnosing adult ADHD on the basis of strict DSM–IV criteria – as well as the above-mentioned methodological difficulties – may lead to underestimation of the prevalence of the disorder in this age group. Thus, further investigations are necessary to find out in what proportion methodological questions or natural developmental features are responsible for the observed decline in the prevalence of ADHD with age. Future well-designed, community-based epidemiological studies critically depend on an improved understanding of the aetiology and pathophysiology of the disorder, which in turn would help to improve the current diagnostic criteria and would thereby facilitate more reliable identification of people with ADHD. We must note that the small number of studies included in the meta-regression analysis and the above-detailed methodological difficulties of the reviewed and analysed studies are also potential limitations of our findings.









eLetters
No eLetters have been published for this article.