In the rich history of speech and language analysis in schizophrenia, researchers have described the errors, structures and meanings in the language of people with schizophrenia, Reference Hoffman, Stopek and Andreasen1–Reference Andreasen and Grove3 focusing on particular symptoms, such as thought disorder, and their manifestation in speech. Reference Hoffman, Stopek and Andreasen1–Reference Andreasen and Grove3 First-person accounts are an invaluable source for increasing empathic understanding; they are not only used in psychiatric training, but are relevant to garnering public awareness. Today, first-person narratives by writers such as Elyn Saks (The Center Cannot Hold Reference Saks4 ) and Kay Redfield Jamison (An Unquiet Mind Reference Jamison5 ) have changed public perceptions of mental illness. However, preconceptions and interpretive frame colour how readers interpret these accounts. Even grounded theory Reference Martin and Turner6 approaches, which purport to draw out themes and meaning, are susceptible to bias, no matter how principled. We thought it would be useful to go back to a more fundamental question: ‘What are the words used?’
There are many ways to attempt to explain how psychotic symptoms arise. In the present study, we tested the hypothesis that, relative to people with mood disorders, people with schizophrenia write with a particular word-use profile reflective of the cognitive disturbances that characterise psychotic symptoms. Cognitive neuroscience models of psychosis focus on the roles of odd perceptual experiences. Reference Kapur7,Reference Corlett, Taylor, Wang, Fletcher and Krystal8 Delusions in particular result from attempts to explain these experiences. Reference Corlett, Taylor, Wang, Fletcher and Krystal8–Reference Kapur11 Those attempts involve disrupted perceptions and inappropriate causal inferences, and are often pervaded with biases, such as external attributions – blaming these odd experiences on outside factors such as other people and out-groups. Reference Corlett, D'Souza and Krystal12 According to one such theory, prediction errors (the mismatches between expectation and experience that drive learning, attentional allocation and belief formation) may be signalled inappropriately in patients with psychosis. Reference Corlett, Murray, Honey, Aitken, Shanks and Robbins13 These aberrant signals drive delusion formation as a means of explaining these odd experiences. We examined whether the key tenets of the cognitive neuroscience frameworks (externalising attributions, aberrant causal inferences, perceptual disturbances) were evident in the written language of patients with schizophrenia compared with those with mood disorder. Our hypotheses were:
-
(a) H1: People with mood disorder use more first-person singular pronouns and affect words. First, as an internal control, we expected, based on prior published work with word counts, Reference Baddeley, Daniel and Pennebaker14 that patients with mood disorder would be self-focused and so would use first-person singular pronouns (‘I’) more frequently than patients with schizophrenia. Given that patients with mood disorder experience pre-dominantly affective symptoms, we also predicted that they would use words describing mood – and particularly some negative mood states – more frequently (i.e. ‘affect’, ‘negative emotions’, ‘sadness’ and ‘anxiety’).
-
(b) H2: People with schizophrenia use more external referents as measured by function word use. Consistent with the external attributions that people with schizophrenia tend to make, we predicted that writers with schizophrenia would use function words (e.g. articles, prepositions, pronouns) that relate to external others (e.g. third-person plural pronouns, hereon referred to as ‘they’) more frequently than patients with mood disorder. We expected that ‘they’ would be enriched relative to third-person singular (‘he’/‘she’), because psychotic symptoms commonly refer to the nefarious intentions of powerful out-groups, Reference Kihlstrom, Hoyt, Oltmanns and Maher15 although there are of course cases of delusions about specific individuals (e.g. the Othello delusion – the delusion that one’s partner is being unfaithful). Reference Miller, Kummerow and Mgutshini16 Also, sense of self is disrupted in phenomenological reports from patients with schizophrenia. Reference Mishara17 We therefore predicted, as in H1, that writers with schizophrenia would use ‘I’ less often than persons with mood disorder.
-
(c) H3: People with schizophrenia use more external referents as measured by content word use. We expected that external attributions would be manifest in content word use – for example words about other humans or human-like agents (e.g. ‘human’, ‘religion’). These predictions are grounded in the cognitive neuroscience of psychotic symptoms, which has demonstrated a bias towards external attributions, consistent with corollary discharge theories of the psychopathology of hallucinations and delusions. In those theories, patients tend to attribute self-generated stimuli and cognitive processes (e.g. motor predictions, inner speech) to external agents. Reference Frith18 We also predicted that less inward focus would manifest as use of fewer content words related to self (e.g. the body) in the writing of people with schizophrenia.
-
(d) H4: People with schizophrenia have different relationships between perceptual and causal words than do people with mood disorder. Early in schizophrenia, patients are over-whelmed by odd experiences that are difficult for them to figure out. This phase of the illness is described as delusional mood. Reference Gross and Huber19,Reference Mishara20 During delusional mood, the world takes on an unexpected and irrepressible significance: it is pregnant with new meaning, significance and salience (Fig. 1). Reference Kapur11,Reference Phillips and Silverstein21–Reference Corlett, Taylor, Wang, Fletcher and Krystal23 Some patients experience an ‘Aha!’ moment Reference Mishara20,Reference Conrad24,Reference Uhlhaas and Mishara25 when a new idea arises to explain their strange unpredictable experiences. The crystallising delusion carries extraordinary explanatory power, diminishing the need for patients to continue their struggle with odd perceptions because the delusion explains them. Reference Kapur11,Reference Gray, Feldon, Rawlins, Hemsley and Smith22,Reference Corlett, Taylor, Wang, Fletcher and Krystal23,Reference Corlett, Honey and Fletcher26–Reference Maher, Oltmanns and Maher29
The profundity of perceptual experience in schizophrenia will likely increase perceptual word use. We had more difficulty predicting how use of words in the Linguistic Inquiry and Word Count category ‘cognitive’ (tentative, certain, causal) might change: patients overwhelmed by confusing perceptual data might use more tentative or circumspect language (e.g. ‘perhaps’), consistent with their uncertain state. They might also use more causal language (‘because’, ‘therefore’, etc.) as they struggle to figure out odd experiences.
In an exploratory analysis, we considered the relationship between perceptual and causal word use across authors. There were at least two possibilities:
-
(a) Perceptual and causal words would be positively correlated: authors in the midst of delusional mood (Fig. 1) might use more causal language as they seek explanations for their aberrantly salient experiences. Reference Kapur11,Reference Gray, Feldon, Rawlins, Hemsley and Smith22
-
(b) Perceptual and causal words would be negatively correlated: once delusions form, people might work less to explain their aberrant experiences, as their delusions are explanatory schema (narratives or world models) for subsequent psychotic experiences (Fig. 1). Reference Mishara and Fusar-Poli9,Reference Jaspers30 Since the authors in our study are publishing essays in a major psychiatric journal, they may be past the chaotic perceptual experiences of early psychosis. We might therefore expect a negative correlation between perceptual and causal word counts.
Method
Text samples
First-person accounts (n = 77; 45 women, 24 men, 8 unclear) describing the experiences of schizophrenia in the ‘First Person Accounts’ section of the journal Schizophrenia Bulletin between 1979 and 2012 were collected. The essays were edited prior to publication, and the authors also noted pre-submission assistance from family, friends and mentors. Sample writers identified themselves as having schizophrenia.
As a non-psychotic psychiatric control group, we collected first-person accounts written by people with mood and anxiety disorders which were published on the internet (n = 29; 19 women, 10 men), mostly on the Anxiety and Depression
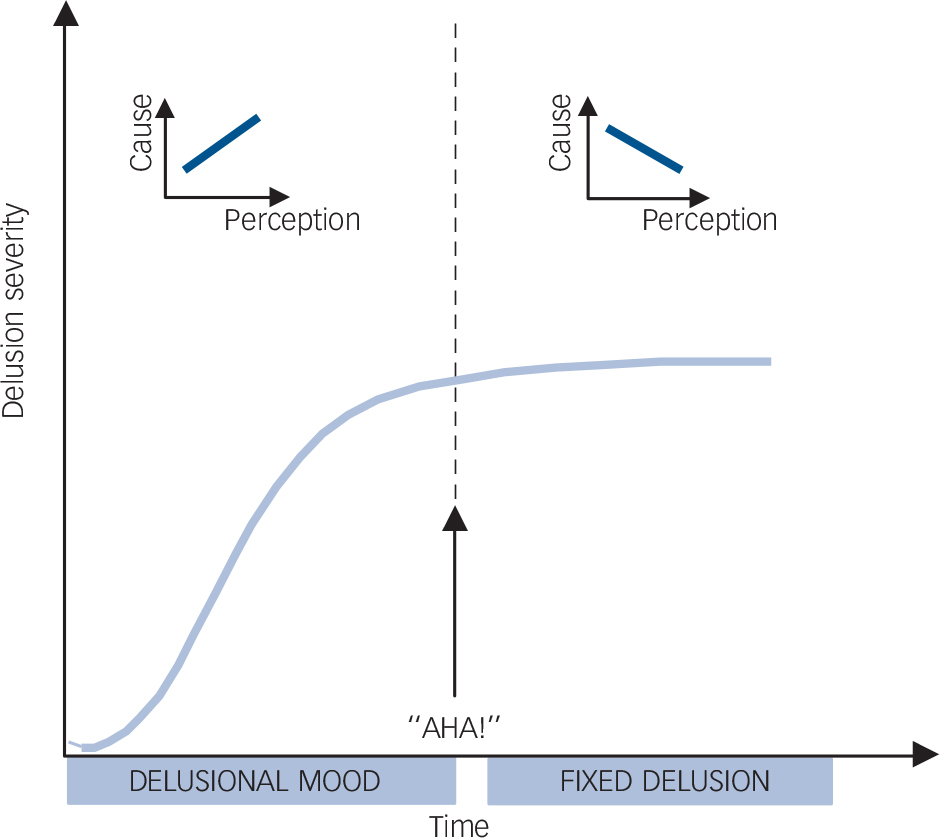
Fig. 1 Model for possible phases of delusion formation and maintenance.
Early in the process, aberrantly salient experiences of the delusional mood provide the impetus for delusions to form. Here, perceptual words and causal words should be positively correlated. Once the delusional explanation is formed, patients report a feeling of insight or an ‘Aha!’ moment in which they arrive at an explanation. Once the explanation has been generated, it becomes a way to organise future experiences, such that perceptual data are sculpted to fit the schema. Hence, the relationship between causal and perceptual language will change, becoming negative.
Association of America (ADAA) website (n = 22/29 samples). The editors of the ADAA website were contacted and they confirmed that the essays were professionally edited. Sample writers identified themselves as having depression, generalised anxiety, panic disorder or obsessive-compulsive disorder. See online Table DS1 for sample details.
Inclusion criteria for all essays were: originally written in English, published after 1975, and written about first-person experience.
Each essay was read by either S.K.F. or S.D-L. for inclusion criteria and processing. Each essay was formatted into a single plain text file using standard procedures, including correcting spelling errors when the intended word was obvious. In addition, we removed quotations longer than two sentences and citations. We placed spaces around dashes and hyphens to separate connected words that were together not recognised by Merriam Webster Dictionary (www.merriam-webster.com). Linguistic Inquiry and Word Count 2007 (LIWC) Reference Pennebaker, Francis and Booth31,Reference Pennebaker, Chung, Ireland, Gonzales and Booth32 – a simple word-counting software – assessed texts for the usage rates of particular word categories. Essays differed in mean length: 2172.55 words (s.e. = 156.31) in schizophrenia and 780.76 words (s.e. = 102.52) in mood disorder essays (F(1,106) = 27.97, adjusted P = 1.15 × 10–5).
Statistics
LIWC reports the percentage of words in each of 68 categories as a function of total words in a text file for function word and content categories. These categories were validated during LIWC development. Reference Pennebaker, Chung, Ireland, Gonzales and Booth32 We considered counts of both function word categories (i.e. words that provide structure in the sentence, such as pronouns and prepositions) and content word categories (i.e. words that indicate topic, such as nouns, regular verbs, and some adverbs and adjectives). One-way ANOVAs were conducted to examine group differences across categories. Reference Pennebaker, Chung, Ireland, Gonzales and Booth32 We determined our significance level to be P<0.05 after false discovery rate (FDR) Reference Benjamini and Hochberg33 correction (based on all 70 compared variables) to reduce the likelihood of Type I error.
Correlations between LIWC’s cognitive and perceptual categories were assessed using bivariate analysis with Pearson’s correlation coefficient (r). Two outliers (with percentages of perceptual words more than two standard deviations above the mean) were removed from this analysis. We determined our significance level to be P<0.05 after FDR correction (based on pairwise comparisons between variables for cognitive mechanisms and variables for perception, 24 possible comparisons). Significant differences between groups in correlations were assessed using Fisher’s r to z transformation.
Results
H1: People with mood disorder use more first-person singular pronouns and affect words
As expected from previous research on word use in samples with mood disorder, our mood disorder sample used ‘I’ more than the schizophrenia sample (Fig. 2) (F(1,106) = 14.45, adjusted P = 2.70 × 10–3). We further found that the mood disorder group used more words to describe affect (F(1,106) = 69.32, adjusted P = 1.18 × 10–11), negative emotion (F(1,106) = 87.45, adjusted P = 1.89 × 10–13), sadness (F(1,106) = 28.38, adjusted P = 1.14 × 10–5) and anxiety (F(1,106) = 82.73, adjusted P = 3.51 × 10–13) (see online Table DS2).
H2: People with schizophrenia use more external referents as measured by function word use
To test our hypothesis that external referents would be greater in schizophrenia, consistent with an external attribution bias, we examined ‘they’. As we predicted, ‘they’ was more frequent (F(1,106) = 12.55, adjusted P = 5.95 × 10–3) in the schizophrenia group relative to the mood disorder group (Fig. 2).
H3: People with schizophrenia use more external referents as measured by content word use
A further test of our prediction about external attribution concerned content word use in schizophrenia. The schizophrenia essays did indeed use significantly more referents to external agents, including more words describing humans (F(1,106) = 7.01, adjusted P = 0.04) (Fig. 3) and religion (F(1,106) = 8.23, adjusted P = 0.02). Consistent with their perturbed sense of self,
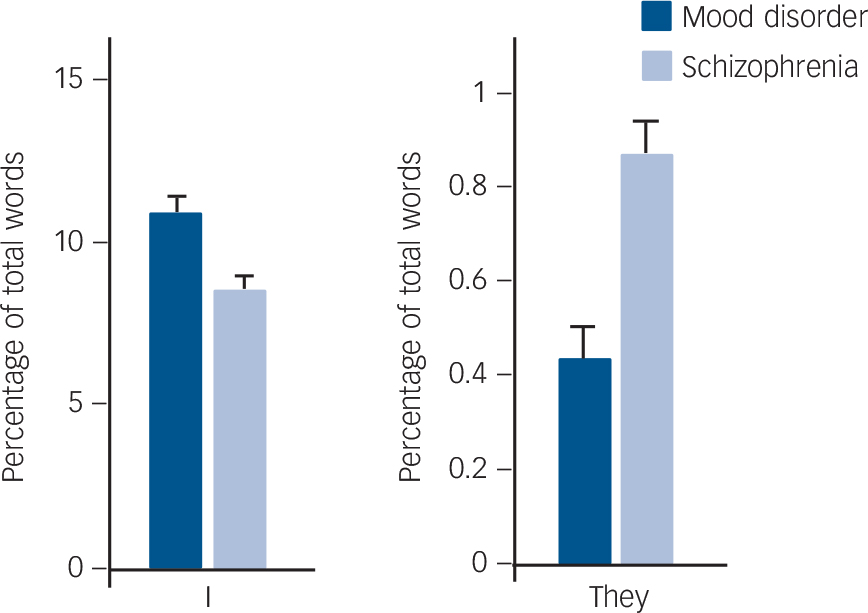
Fig. 2 Use of function words by the mood disorder and schizophrenia groups.
Writers with schizophrenia used the first-person singular pronoun (‘I’) less frequently and the third-person plural pronoun (‘they’) more frequently than did writers with mood disordes. Bars represent mean value and error bars represent standard error.
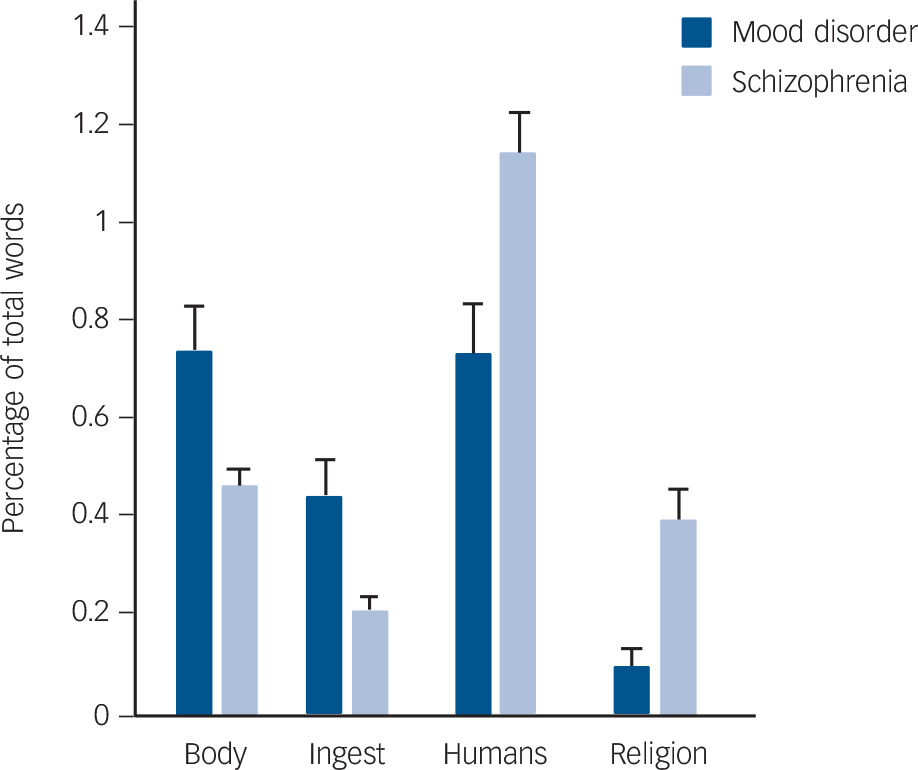
Fig. 3 Use of content words by the mood disorder and schizophrenia groups.
Writers with schizophrenia used words describing the body and ingestion less and words describing humans and religion more then did writers with mood disorders. Bars represent mean value and error bars represent standard error.
patients with schizophrenia used fewer words describing the body (F(1,106) = 11.86, adjusted P = 7.52 × 10–3) and ingestion (F(1,106) = 11.44, adjusted P = 7.79 × 10–3).
H4: People with schizophrenia have different relationships between perceptual and causal words than do people with mood disorder
Next, we examined the essays for differences in perceptual and causal language. We did not observe a significant difference in perceptual words. However, both causal language (F(1,106) = 9.45, adjusted P = 0.016) and tentative language (F(1,106) = 8.30, adjusted P = 0.020) were less frequent in the schizophrenia essays than in the mood disorder essays (Fig. 4).
We predicted that aberrant salience and subsequent causal inference in schizophrenia Reference Corlett, Murray, Honey, Aitken, Shanks and Robbins13 might manifest in written language as a correlation between perceptual and causal words. We computed Pearson’s correlation between these two categories as measured by LIWC. We found that causal and perceptual words were significantly negatively correlated in the schizophrenia essays (r = –0.276, FDR adjusted P = 0.02) (Fig. 4), and significantly positively correlated in the mood disorder essays (r = 0.524, FDR adjusted P = 0.02). These correlations were significantly different between the two groups (Fisher’s z-transformed r = 3.29, P = 2 × 10–4).
Post-hoc analyses
To test whether any of the differences between the two groups were influenced by differences in essay length (as measured by word count), we conducted a MANCOVA on the 12 variables described earlier, with word count as a covariate. The two groups were significantly different (Wilk’s lambda test, F(1,12) = 10.94, P = 3.43 × 10–13). The subsequent ANCOVAs with word count as a covariate for each variable revealed that word count significantly altered the result only for affect (F(1,12) = 9.76, P = 0.002, partial eta squared = 0.09). All between-group differences remained statistically significant after FDR correction (adjusted P<0.05) for all 12 variables (details in online Table DS3).
To test whether the differences between the correlations in causal and perceptual words for the two groups (H4) were
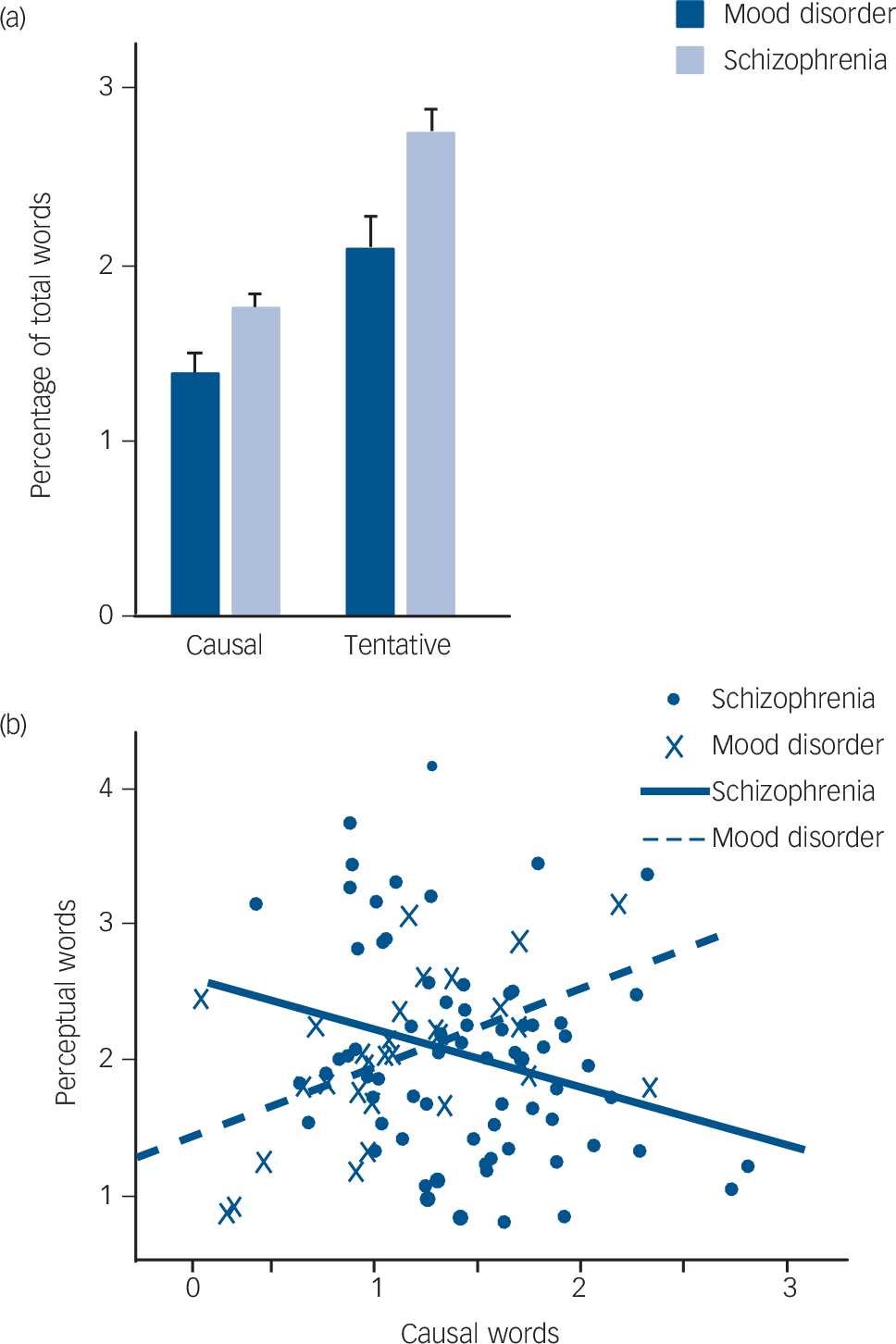
Fig. 4 (a) Use of causal and tentative words by the mood disorder and schizophrenia groups (bars represent mean value; error bars represent standard error) and (b) percentage of words describing perception and causality by the two groups (data points represent values in individual essays; lines represent linear fit).
influenced by differences in essay length, we conducted partial correlations with word count as a covariate. The observed correlations between causal and perceptual words remained significant for mood disorder essays (r = 0.546, adjusted P = 0.003) and for schizophrenia essays (r = –0.356, adjusted P = 0.002).
Discussion
We used a computerised text-analysis approach to examine word use in schizophrenia. Our work extends previous findings in language and psychology to suggest that psychiatric patients with different diagnoses (psychotic illness v. mood disorder) use language differently, not just in what they say (as marked by content words), but in how they say it (as marked by function words). Reference Chung, Pennebaker and Fiedler34
Schizophrenia accounts differ in affective expression relative to mood accounts
Function words are known to differ between individuals enough to profile the demographics and personality of authors Reference Stamatatos35 to identify the authors behind pen names and terrorist threats Reference Juola36 (for a review, see Stamatatos Reference Stamatatos35 ). Using LIWC, function word use was found to differ in some psychiatric conditions; for example, ‘I’ is used more by people with depression than healthy controls, indicating greater inward focus. Reference Baddeley, Daniel and Pennebaker14,Reference Stirman and Pennebaker37,Reference Rude, Gortner and Pennebaker38 Also, Junghaenel et al Reference Junghaenel, Smyth and Santner39 applied LIWC to language samples from 27 psychiatric and 17 control patients. In this mixed psychiatric group (which included many patients with psychosis), there were significant differences between groups in language describing positive emotions, cognitive processes and relativity. Furthermore, others have established that the relationships between the types of words used may be different in patients with psychosis. Specifically, using acyclic speech graphs to analyse speech from patients with schizophrenia and bipolar disorder, Mota and colleagues found evidence for verbosity and flight of thoughts in patients with mania. Reference Mota, Vasconcelos, Lemos, Pieretti, Kinouchi and Cecchi40 In the present study, we replicated the higher rates of first-person singular pronouns and negative affect word use associated with depression in our writers with mood disorder. Reference Baddeley, Daniel and Pennebaker14,Reference Stirman and Pennebaker37,Reference Rude, Gortner and Pennebaker38
Schizophrenia accounts use more external referents as measured by function word use relative to mood accounts
We examined word use in writing by people with schizophrenia and those with mood disorder to test the hypothesis that it would accord with cognitive neuroscience models of psychopathology, such as the prediction error model of delusions Reference Corlett, Murray, Honey, Aitken, Shanks and Robbins13 and the corollary discharge theory of disturbed self-agency. Reference Frith18 Indeed, writers with schizophrenia used ‘they’ significantly more than writers with mood disorder. We suggest that this is consistent with the externalising bias observed in cognitive neuroscience studies of patients with schizophrenia. Reference Keefe, Arnold, Bayen, McEvoy and Wilson41 It may also reflect a shift in people with schizophrenia towards thinking of self as other. Reference Mishara17
Schizophrenia accounts use more external referents as measured by content word use relative to mood accounts
External bias was also present in the content words used by people with schizophrenia. They wrote with significantly less self-focus (reflected in less talk of the body and ingestion), and they used words about external others (human agents and religion) more. These differences might reflect a mix of explanatory inference and coping. People with psychosis misattribute internally generated processes (e.g. thoughts) to external sources (e.g. the US Central Intelligence Agency (CIA), angels or demons), perhaps because of an attenuated forward model of self, generating surprising experiences that individuals without psychosis would normally disregard. Reference Corlett, Frith and Fletcher42 Such experiences are distressing and alienating. Religious practice and social relationships can help patients with psychosis find a sense of community and belonging.
Schizophrenia accounts have different relationships between perceptual and causal words than do mood accounts
We also found that the schizophrenia essays differed significantly from the mood disorder essays in the use of causal and tentative words, and in the direction of correlation between perceptual and causal words (negative in schizophrenia and positive in mood disorders). It could be that the language used by patients with schizophrenia reflects their phase of illness (see Fig. 1, delusional mood and fixed delusion phases). Early aberrant experiences require explanation, Reference Kapur11,Reference Corlett, Murray, Honey, Aitken, Shanks and Robbins13,Reference Corlett, Taylor, Wang, Fletcher and Krystal23,Reference Corlett, Frith and Fletcher42–Reference Sass46 which would lead to increased causal words (e.g. ‘because’) at the same time as words about their perceptions (positive correlation). After delusions crystallise, patients no longer seek explanations for their odd experiences (they now rely on their delusion to do explanatory work), Reference Jaspers30 so they talk less about the reasons when they describe their experiences (negative correlation). Reference Corlett, Krystal, Taylor and Fletcher44 We found a negative correlation, consistent with our authors being further along in their illness and outside of the delusional mood. To be in our group, they have had symptoms for long enough to receive a diagnosis of schizophrenia, and to accept it enough to write as a person with the disorder. We expect that in this post-‘Aha!’ phase, people use the explanation (delusion) as a perceptual schema – a filter through which subsequent perceptual data are viewed – ‘the trail is blazed and the now dominant delusion motivates future apperceptive schema’. Reference Jaspers30 Confirmation biases and a general tendency towards dogmatism in the face of contradictory evidence prevail (in everyone, not just people with psychosis Reference Kelly47 ). Once we endorse a belief, our relationship to evidence changes. We are more likely to refute or ignore evidence than to relinquish a cherished belief or generate a new explanation Reference Kelly47 (think here not only of patients, but also of scientists). Reference Corlett, Taylor, Wang, Fletcher and Krystal23,Reference Maher, Oltmanns and Maher29
There was a positive correlation between perceptual and causal words in the mood disorder group. Some studies find that people with mood disorder are less prone to the biases that attend causal inference; they show depressive realism. Reference Dobson and Franche48 For example, they do not have an illusory sense of control of non-contingent positive outcomes. However, controls without mood disorder and patients with psychosis felt they were in control when they were not. Reference Bentall and Kaney49 In the absence of benefactance biases, people with mood disorder may make a more straightforward connection between perception and causation, and so be more likely to use them together.
Other factors likely modulate patients’ talk of both perception and causality. In-patients with schizophrenia and delusions do not report more current anomalous percepts than do psychiatric controls without psychosis. Reference Bell, Halligan and Ellis50 This may be because treatment works: antipsychotic drugs attenuate aberrantly salient experiences. Reference Mizrahi, Kiang, Mamo, Arenovich, Bagby and Zipursky51 However, patients also learn quickly that talking less about odd experiences and ideas can lessen unwanted clinical attention and unpleasant social interactions. Reference Haddock, Tarrier, Spaulding, Yusupoff, Kinney and McCarthy52 They may learn to alter what they say about their experiences.
The attenuation of aberrant salience by antipsychotic drugs Reference Mizrahi, Kiang, Mamo, Arenovich, Bagby and Zipursky51 could disconnect perception and belief, encouraging the adoption of alternative non-delusional explanations. Reference Corlett, Krystal, Taylor and Fletcher44,Reference Gottlieb, Cather, Shanahan, Creedon, Macklin and Goff53 In fact, some recovering patients actually report a kind of double awareness, where they believe and do not believe their delusions. Reference Stanton and David54 Presumably this too would change the correlation between perceptual and causal word use.
Future work will help to clarify which, if any, of these explanations holds. Further investigations of spontaneous language across phases of illness and recovery will be critical.
Limitations
The text samples for both disorders may have been edited before publication and perhaps lost some of their original voice and vocabulary through this process. The extent of editing may have been uneven both within and across groups: we did not have access to the unedited initial drafts during the development of this project. Future work with un-edited language samples may identify a broader signature of language changes specific to people with schizophrenia. The schizophrenia and mood disorder essays came from different sources, and although they were on the same topic (‘what it is like to live with my mental illness’), this may contribute to differences. Also, the mood disorder essays were mostly directed at other patients (v. schizophrenia essays published in an academic medical journal mostly read by health professionals) and were on average half the length.
We cannot confirm diagnosis or symptomatology of the authors whose essays we included in this project. The authors in the schizophrenia group may have comorbid mood disorder and the authors in the mood disorder group may have psychotic symptoms. Furthermore, the authors of the schizophrenia essays may represent a particularly functional group of people with schizophrenia, as they are aware of this medical journal and have written and submitted essays. Indeed, some are even peer professionals and scientists with lived experience of psychosis Reference Chadwick55 who provide a uniquely relevant perspective on cognitive and neuroscientific approaches to their symptoms. Reference Chadwick55
However, having read the essays, we are certain that most patients’ accounts were not explicitly discussing cognitive neuroscience and that the findings we report reflect the impact of illness mechanisms on language. Importantly, we did note that some language features in these essays that have been previously observed in patients with schizophrenia: the schizophrenia essays included several neologisms (Table DS1) whereas the mood disorder essays contained none. Reference Covington, He, Brown, Naci, McClain and Fjordbak56 We also suspect that the observation of fewer punctuation marks in the schizophrenia essays may represent a disorganised quality of the language. Reference Bruthiaux57
Finally, we note the lack of a non-psychiatric control group. Such a sample would increase our confidence in the direction of our findings – did the people with schizophrenia use ‘I’ less or were the people with mood disorder using it more? We made a priori predictions, based on prior data; future work will seek out an appropriate comparison group.
Directions for future work
Future work will establish the relationships between the language markers identified presently and the behavioural and neural markers of disrupted learning and inference identified previously. Reference Corlett, Murray, Honey, Aitken, Shanks and Robbins13 It will be informative to sample language use across illness course as delusions form and become engrained and resistant to change. Reference Corlett, Krystal, Taylor and Fletcher44 We will also consider people with different symptom dimensions and disease severity. Indeed, we aim in the future to use the written and spoken language of patients with schizophrenia to classify patients not simply into diagnostic categories, but to take a more dimensional approach to specific symptoms – such as delusions – and use language as another means of testing theoretical models of underlying pathology – much like the Research Domain Criteria initiative which the National Institutes of Health have put forth as a way to reorganise pathological categories based on data-driven dimensions. Reference Insel, Cuthbert, Garvey, Heinssen, Pine and Quinn58
We also expect that additional computational tools will allow us to delve deeper into text features, such as proximity of word types of interest and proposition density. Reference Covington, He, Brown, Naci, McClain and Fjordbak56
Implications
We were able to identify differences in the writing of patients with schizophrenia as compared with patients with mood disorder. Some of these patterns of language use may actually be relevant to the pathophysiology of symptoms. There is clearly more work to do, but we feel this is an important first step towards a more data-driven understanding of what our patients are trying to tell us.
Acknowledgements
We would like to thank the STEP discussion group for inspiring discussion of psychosis and specific feedback on this project. Also, Marc Briel contributed to early analyses, Adam Mecca helped with counting of neologisms, and John Strauss and James W. Pennebaker commented on earlier drafts of the manuscript.









eLetters
No eLetters have been published for this article.