Depression is an important public health problem, and one of the leading causes of disease burden worldwide. Reference Murray and Lopez1 The Medical Outcomes Study collated data from 11 242 out-patients in the USA and showed that depressive symptoms, with or without major depressive disorder, impaired functional ability and well-being as much as the most common chronic medical conditions such as diabetes, chronic lung disease, hypertension and heart disease. Reference Wells, Stewart, Hays, Burnam, Rogers and Daniels2,Reference Wells, Burnam, Rogers, Hays and Camp3 After 2 years of follow-up around 40% of those with major depression were still affected and functionally impaired, whereas those with chronic minor depression (dysthymia) had the worst outcome. Most had only partial recovery of functional ability. Reference Wells, Burnam, Rogers, Hays and Camp3 Primary care populations with chronic or recurrent depression, although clinically important, are rarely investigated as a distinct patient group. Reference Conradi, de Jonge and Ormel4 It is known that chronicity of depression is associated with high mortality, greater psychological and social morbidity and high use of primary care services, Reference Lloyd, Jenkins and Mann5 but there is little consistency regarding longer-term management of this disorder. Reference Arroll and Moir6 Studies from the USA indicate that organised, enhanced care can have a beneficial effect on outcomes for patients with acute major depression, Reference Katon, Robinson, Von Korff, Lin, Bush and Ludman7 and also those with persistent depression Reference Simon, Katon, VonKorff, Unützer, Lin and Walker8 or at high risk of recurrence. Reference Katon, Rutter, Ludman, von Korff, Lin and Simon9 However, there are increased costs associated with such an approach and beneficial effects can decline over time, such that a longer-term approach may be indicated, particularly for those with chronic difficulties. Reference Rost, Nutting, Smith, Elliott and Dickinson10 Most people with depression are treated in primary care, but there have been few trials of interventions targeted at those with chronic or recurrent depression in either primary or secondary care settings, with most examining interventions for newly diagnosed depression. Reference Gilbody, Bower, Fletcher, Richards and Sutton11 Collaborative care models include specialist input, which is potentially more costly to deliver than models based solely in primary care. Given the associated unmet needs, significant morbidity and costs there is a need for new approaches to management of this problem in primary care. The aim of this trial was to evaluate the management of chronic depression with regular structured proactive contact and follow-up of patients by practice nurses over 2 years, supported by general practitioners (GPs) as compared to usual GP care.
Method
Study design and participants
This was a randomised controlled trial (RCT) (the ProCEED trial, registered at Current Controlled Trials: ISRCTN36610074) comparing GP ‘usual care’ (control), with a ‘proactive care’ approach involving regular follow-up by practice nurses (intervention) in addition to GP usual care, for patients with recurrent or chronic depression (see protocol paper for details Reference Buszewicz, Griffin, McMahon, Beecham and King12 ). Participants were recruited from 42 general practices throughout the UK. All participants gave written, informed consent. Ethics approval was given by the Royal Free Hospital Ethics Committee – REC reference number 07/Q0501/15.
Inclusion criteria were:
-
(a) adults aged 18 and over;
-
(b) two or more documented episodes of major depression within the previous 3 years;
-
(c) evidence of recurrent and/or chronic depression via the Composite International Diagnostic Interview (CIDI, lifetime) questionnaire Reference Kessler, Abelson, Demler, Escobar, Gibbon and Guyer13 (chronic depression was categorised as an episode of major depression lasting at least 2 years within the 3 years prior to recruitment or chronic dysthymia for the 2 years prior to recruitment);
-
(d) a baseline Beck Depression Inventory (BDI-II) score of 14 or above; Reference Arnau, Meagher, Norris and Bramson14
-
(e) sufficient English to be able to complete self-report questionnaires.
Exclusion criteria were:
-
(a) current psychotic symptoms;
-
(b) impaired cognitive function;
-
(c) incapacitating alcohol or drug dependence.
Consent and randomisation
After a thorough explanation of the study to potential participants, written informed consent was obtained from those fulfilling the inclusion criteria and agreeing to take part. Consenting participants were individually randomised by telephone, using the independent Medical Research Council (MRC) computerised randomisation service and a blocked design to maintain a balance of numbers in control and intervention groups. All participants completed baseline questionnaires at the practice prior to being informed about their randomisation result by the research nurse. All study team members apart from the project manager were masked to block size and group allocation.
Trial intervention
The intervention, termed ‘proactive’ care, involved regular scheduled follow-up appointments with trained nurses over the 24 months of the trial. The intervention group had a baseline assessment and further sessions were offered after 1 month, 2 months later and then every 3 months for the remainder of the 2 years of the trial, i.e. a total of 10 appointments. Most were face to face, although patients had the option to elect for telephone appointments when attending the surgery was difficult. A joint management plan was formulated between the nurses and each of their patients at the baseline assessment and reviewed during subsequent appointments. If clinically indicated the reviews could be more frequent and if nurses were concerned about a patient, they were asked to discuss them with the relevant GP, who might also see the patient if indicated.
At each session the nurses asked about the patients' current mood and reviewed their social circumstances, current treatment (medication and/or psychological therapy), and any side-effects. They discussed participants' queries about current or past treatments and checked their concordance with treatment, clarifying any reasons for poor concordance. If there were current symptoms of depression, alternative or additional treatments were discussed. The nurses were given brief training in problem-solving and motivational interviewing techniques Reference Mynors-Wallis, Gath, Day and Baker15,Reference Rollnick, Heather and Bell16 and used these to help the participants to identify their own problems, solutions, motivation for change and preferences for care.
The intervention was manualised and has been described in detail elsewhere. Reference Buszewicz, Griffin, McMahon, Beecham and King12 All participating nurses received at least one quality assurance visit from a senior, independent MRC GP research framework training nurse. The intervention group were also given an educational booklet designed for the trial, which included information about depression and that outlined current evidence-based thinking about its treatment (the intervention manual and educational booklet are obtainable on request from the authors).
Nurse training and clinical supervision sessions
The research team provided 3 days' training for all participating practice nurses. Reference Buszewicz, Griffin, McMahon, Beecham and King12 A further day's training was provided for nurses conducting the outcome assessments. Each nurse was assigned a member of the research team as a ‘clinical supervisor’ (two were GPs with an interest in mental health and one a clinical psychologist). Nurses had telephone contact every 3–4 months with their supervisors and could contact them in between with any patient concerns.
Control arm
Participants in the control group received ‘treatment as usual’ and continued to see their GP on request. They did not see the practice research nurse for any mental health intervention.
Outcome measures
The outcome measures were as follows:
-
(a) the primary outcome measure was the BDI-II; Reference Arnau, Meagher, Norris and Bramson14
-
(b) functional impairment was measured using the Work and Social Activity Scale (WSAS); Reference Mundt, Marks, Shear and Greist17
-
(c) DSM-IV diagnosis and frequency of depressive episodes assessed using the CIDI questionnaire Reference Kessler, Abelson, Demler, Escobar, Gibbon and Guyer13 at recruitment and follow-up;
-
(d) health-related quality of life measured using the EuroQuol EQ-5D. Reference Brooks18 Here we report results from the visual analogue scale (EQ-VAS);
-
(e) practice service data on number of GP visits, practice nurse contacts, referrals for psychological therapy and prescriptions for psychotropic medication collected for 24 months before recruitment and the 24 months of the trial.
The BDI-II was completed at baseline, 3, 6, 12, 18 and 24 months by self-complete questionnaire. All other measures were collected at baseline and 24 months. Reference Buszewicz, Griffin, McMahon, Beecham and King12 The CIDI was completed face to face with a practice research nurse at baseline and 2 years. Final assessment interviews were conducted by research nurses not involved in delivering the intervention who were masked to participants' trial group allocations. As a check on masking they were asked to estimate which trial arm each participant had been randomised into. Practice service-use data were collected by practice nurses involved in the initial recruitment and delivery of the intervention. All other outcome measures were obtained by self-complete questionnaires.
Sample size and statistical analysis
Data were double entered and analysed using SPSS for Windows release 15.0 and Stata release 10. The sample size was calculated to detect a clinically important difference in BDI-II at 90% power and the 5% (two-sided level) of significance. A pooled standard deviation of 11.0 was assumed and the sample sizes adjusted for clustering using an intraclass correlation (ICC) of 0.02. Reference King, Davidson, Taylor, Haines, Sharp and Turner19 For a 4-point difference in BDI (assuming an average 10 patients per practice) the required sample size would be 376. Reference Buszewicz, Griffin, McMahon, Beecham and King12 Thus 38 practices with 10 patients per practice (total 380) would meet the required sample size. To take account of possible attrition, recruiting 12–14 patients per practice would allow for 25% attrition, meaning a total of 532 participants would be required.
For continuous variables, means and standard deviations were calculated, and for categorical variables, numbers and percentages. All analyses were undertaken on an intention-to-treat (ITT) basis. For the primary (BDI-II) and secondary (WSAS and EQ-VAS) outcomes we used multilevel modelling adjusted for clustering by general practice. Reference Rabe-Hesketh and Skrondal20 For the BDI-II the multilevel modelling included an additional level to take account of repeated measures over time. All models fitted reflected the appropriate hierarchical structure of the data and adjusted for baseline values of the relevant outcome. Practice service-use data were analysed using analysis of covariance (ANCOVA), adjusting for baseline values and using robust standard errors to account for clustering. Reference Vickers and Altman21
To calculate the effect sizes of the main outcome measures we used a method utilising estimates derived from the multilevel models (Hedge's g). Reference Hedges22 For the BDI-II, WSAS and EQ-VAS the effect of number of ‘nurse sessions’ attended on outcome was also assessed using a contamination-adjusted ITT analysis. Reference Sussman and Hayward23 This was implemented using instrumental variable regression with the 24-month follow-up score as the outcome, randomisation as the instrumental variable, baseline score and number of sessions as explanatory variables and robust standard errors to take account of clustering. A contamination-adjusted ITT analysis allows adjustment for non-adherence, avoiding the biases of as treated and per-protocol analyses and preserving the randomness of allocation by examining how control patients ‘would have’ behaved were they to have been in the experimental arm. It is similar in principle to a complier average causal effect analysis.
Results
We approached 3293 potentially eligible people from 42 general practices throughout the UK, identified predominantly from practice-database searches. Participants were recruited between November 2007 and July 2008 and the 2-year follow-up continued until the end of July 2010. Of 3293 people initially approached, 959 (29%) expressed an interest in attending for interview and 828 (25%) attended. Following the recruitment interview and assessment 558 people were found eligible and agreed to take part (Fig. 1).
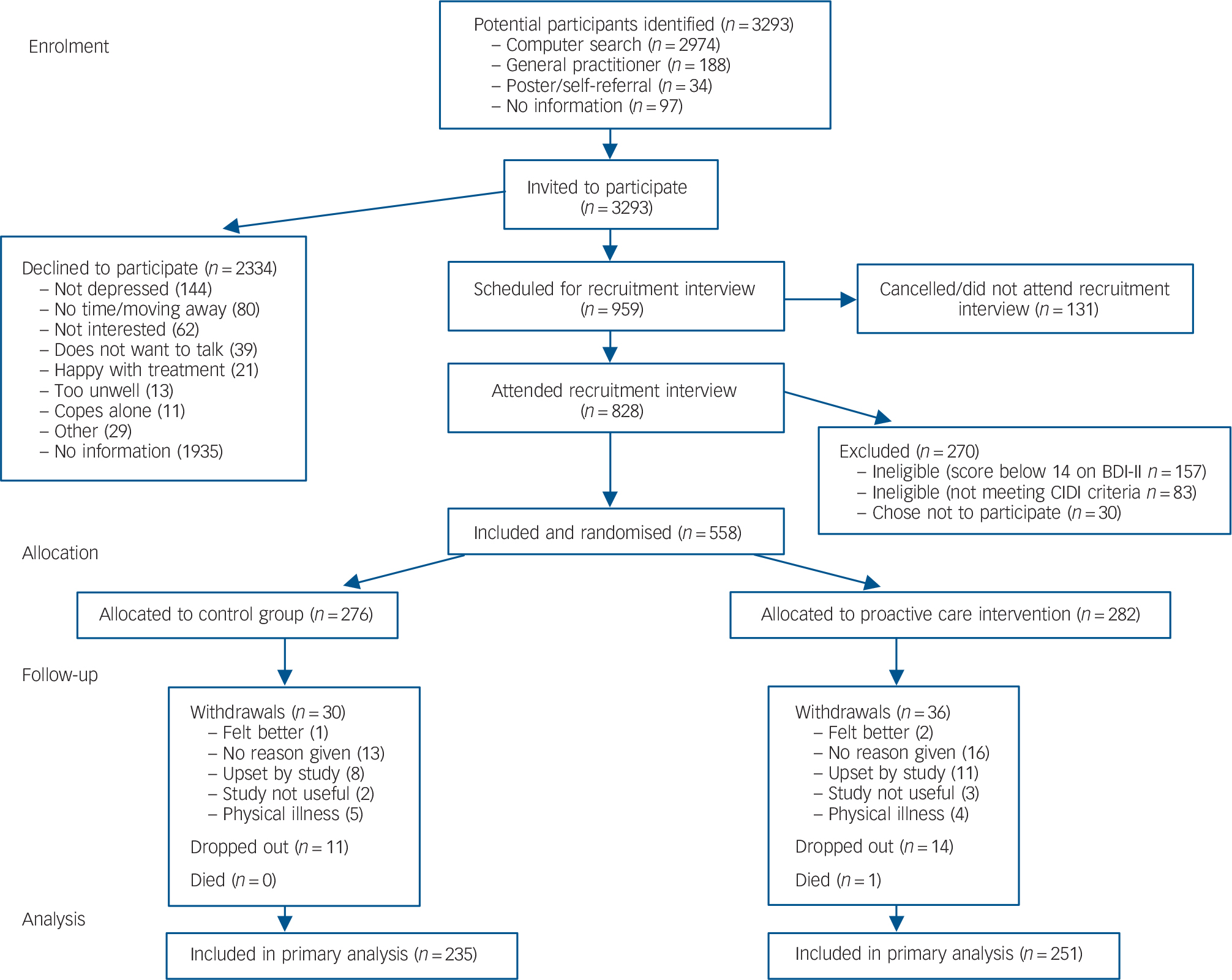
Fig. 1 Consort diagram: recruitment and treatment group allocation.
BDI, Beck Depression Inventory; CIDI, Composite International Diagnostic Interview.
Participants' questionnaire responses for the primary outcome, the BDI-II, were: 99% at baseline; 72% at 3 months; 66% at 6 months; 66% at 12 months; 62% at 18 months and 78% at 24 months. Because of concern about attrition between 3 and 6 months, following discussion at the Trial Steering Group and having obtained ethical approval, we incentivised the return of questionnaires from the 12-month follow-up point with £10 shopping vouchers. Reference Edwards, Roberts, Clarke, DiGuiseppi, Wentz and Kwan24
The 24-month outcome interviews were completed face to face with a different research nurse from the nurse conducting the initial recruitment and intervention and participant response was 65%. A further 13% of participants returned the final BDI-II by post. A total of 66 participants (12% of the total) formally withdrew over the 24 months of the study; 36 in the intervention group and 30 in the control group. One participant in the intervention group died of cancer during the trial.
Of the 282 participants in the intervention group, 77 (27%) were poor attenders and only attended 0–4 intervention sessions, 83 (29%) were moderate attenders and attended 5–8 sessions and 122 (43%) were good attenders, having attended 9–11 intervention sessions. The latter group were considered to have attended for the full intervention as various timing constraints meant that not all could be offered the full 10 sessions initially intended.
Baseline characteristics
The two groups were well balanced with respect to baseline characteristics, with no large differences between the intervention and control groups (Table 1).
Table 1 Baseline sociodemographic characteristics, diagnoses, symptoms, function and health services utilisation a

| Intervention group |
Control group |
Intervention group, n |
Control group, n |
|
|---|---|---|---|---|
| Age, years: mean (s.d.) | 48.3 (12.3) | 48.4 (13.4) | 282 | 276 |
| Women, n (%) | 217 (77.0) | 201 (72.8) | 282 | 276 |
| Married, n (%) | 133 (47.7) | 127 (46.9) | 279 | 271 |
| Living with partner/children, n (%) | 212 (76.3) | 188 (69.1) | 278 | 272 |
| Accommodation, owner-occupied, n (%) | 188 (68.6) | 179 (66.1) | 274 | 271 |
| Ethnicity, White: n (%) | 251 (90.6) | 241 (89.3) | 277 | 270 |
| Paid employment, n (%) | 137 (48.9) | 121 (44.8) | 280 | 270 |
| Diagnosis (Composite International Diagnostic Interview), n (%) | 278 | 272 | ||
| Chronic major depression | 78 (28.1) | 86 (31.6) | ||
| Recurrent depression | 155 (55.8) | 142 (52.2) | ||
| Dysthymia | 45 (16.2) | 44 (16.2) | ||
| Beck Depression Inventory-II, mean (s.d.) | 31.9 (9.8) | 33.1 (10.6) | 278 | 272 |
| Work and Social Activity Scale, mean (s.d.) | 22.1 (9.6) | 22.4 (9.4) | 280 | 272 |
| Euroquol Visual Analogue Scale, mean (s.d.) | 54.5 (19.5) | 52.8 (20.1) | 281 | 269 |
| General practitioner visits, mean (s.d.) | 15.5 (9.9) | 15.8 (9.7) | 270 | 271 |
| General practitioner home visits, mean (s.d.) | 0.2 (1.2) | 0.2 (0.9) | 236 | 224 |
| Practice nurse visits, mean (s.d.) | 3.9 (4.7) | 4.5 (5.1) | 258 | 254 |
| Practice counsellor visits, mean (s.d.) | 0.7 (2.6) | 0.4 (1.4) | 258 | 254 |
| Referrals to psychological therapy/psychotherapy, mean (s.d.) | 0.4 (0.9) | 0.3 (0.6) | 155 | 145 |
| Referrals to psychiatrist/community mental health team, mean (s.d.) | 0.4 (0.7) | 0.6 (1.8) | 154 | 154 |
| Number of months on antidepressants, mean (s.d.) | 14.1 (8.8) | 12.7 (8.3) | 267 | 269 |
a. Service-use data refers to the 24 months prior to the baseline assessment.
Outcome results at 24 months
Primary outcome
Scores for the BDI-II at follow-up improved (decreased) in both groups over time (Table 2). There was a small but not significantly greater improvement in the intervention group. The estimated average difference in score, from the multilevel modelling, was lower (i.e. better) by 1.2 (95% CI −0.3 to 2.7, P = 0.125) in the intervention group when accounting for all time points.
Table 2 Beck Depression Inventory-II scores across follow-up times

| 3 months | 6 months | 12 months | 18 months | 24 months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (s.d.) | n | Mean (s.d.) | n | Mean (s.d.) | n | Mean (s.d.) | n | Mean (s.d.) | |
| Control group | 180 | 29.2 (12.8) | 167 | 28.8 (13.8) | 166 | 27.9 (13.6) | 152 | 27.3 (13.6) | 206 | 26.0 (14.9) |
| Intervention group | 221 | 28.1 (12.3) | 201 | 25.8 (12.7) | 201 | 25.2 (12.8) | 196 | 25.1 (14.4) | 224 | 22.1 (14.2) |
Secondary outcomes
Summary results at 24 months are presented in Table 3. From the multilevel modelling, the WSAS score was found to be significantly lower (i.e. better) by 2.5 (95% CI 0.6 to 4.3, P = 0.010) in the intervention group at 24 months and the EQ-VAS score was higher (i.e. better) by 2.9 (95% CI −0.8 to 6.5, P = 0.127) in the intervention group at 24 months.
Table 3 Outcomes at 24-month follow-up a

| Intervention group |
Control group |
Intervention group, n |
Control group, n |
|
|---|---|---|---|---|
| Work and Social Activity Scale, mean (s.d.) | 16.2 (12.1) | 18.8 (12.1) | 224 | 205 |
| Euroquol Visual Analogue Scale, mean (s.d.) | 61.7 (21.6) | 58.0 (21.4) | 214 | 201 |
| General practitioner visits, mean (s.d.) | 13.7 (9.5) | 13.4 (9.1) | 234 | 226 |
| General practitioner home visits, mean (s.d.) | 0.1 (0.6) | 0.1 (0.5) | 193 | 190 |
| Practice nurse visits, mean (s.d.) | 5.5 (6.6) | 4.8 (6.6) | 234 | 226 |
| Practice counsellor visits, mean (s.d.) | 0.7 (2.1) | 0.4 (1.6) | 234 | 226 |
| Referrals to psychological therapy/psychotherapy, mean (s.d.) | 0.6 (1.2) | 0.3 (0.6) | 133 | 119 |
| Referrals to psychiatrist/community mental health team, mean (s.d.) | 0.6 (1.4) | 0.4 (0.8) | 117 | 126 |
| Number of months on antidepressants, mean (s.d.) | 13.6 (9.7) | 11.7 (9.6) | 261 | 250 |
| Diagnosis (Composite International Diagnostic Interview), n (%) | 196 | 169 | ||
| Chronic major depression | 27 (13.8) | 28 (16.6) | ||
| Recurrent depression | 87 (44.4) | 60 (35.5) | ||
| Dysthymia | 25 (12.8) | 27 (16.0) | ||
| No episodes of depression | 57 (29.1) | 54 (32.0) | ||
a. Service-use data refers to the 24 months prior to the 24-month follow-up assessment.
The only statistically significant differences in service use were for practice nurse visits and number of months on antidepressants. Both were higher in the intervention group, with adjusted mean differences (intervention–control) of 1.6 (95% CI 0.2 to 3.0, P = 0.026) and 1.4 (95% CI 0.02 to 2.8, P = 0.047) respectively. A comparison of the proportions in each diagnostic category (CIDI) between intervention and control groups at follow-up showed no statistically significant difference (P = 0.368).
Effect sizes and contamination-adjusted ITT analysis
Using Hedge's g method gave us the effect sizes: BDI-II = 0.09; WSAS = 0.21; EQVAS = 0.14. Results investigating the effect of the number of intervention sessions on BDI-II, WSAS and EQ-VAS scores using the contamination-adjusted ITT analysis showed the following ‘per nurse treatment-session’ effects on average score: BDI-II (−0.37, 95% CI −0.68 to −0.07, P = 0.017), WSAS (−0.33, 95% CI −0.55 to −0.10, P = 0.004) and EQ-VAS (0.38, 95% CI −0.13 to 0.88, P = 0.142), indicating statistically significant improvements (decreases) per session in BDI-II and WSAS scores of −0.37 and −0.33 respectively. We then multiplied the per session effect by the number of sessions attended, which would lead to a reduction in BDI-II score of 3.7 points and a reduction in WSAS scores of 3.3 points more in the patients in the intervention group than controls if all 10 intervention sessions were attended. This assumes from the analysis that each session is likely to have the same effect on outcome and thus the effect of the sessions attended is additive.
Masking of the final assessment
Agreement between the trial arm allocation and guesses of the research nurses undertaking the final patient assessment (n = 361) was low (kappa (κ) = 0.281, P<0.001), indicating successful masking of the outcome assessments.
Discussion
Principal findings
There was no significant improvement in depression score (BDI-II) or quality of life (EQ-5D) at 24-month follow-up in the overall sample, but there was an improvement in social functioning (WSAS). The contamination-adjusted ITT analysis, conducted to assess the effect of the number of sessions received, demonstrated a positive per session effect for both BDI-II and WSAS scores. From this contamination-adjusted ITT analysis it could be inferred that patients attending all 10 intervention sessions might be expected to reduce their BDI-II score by 3.7 points more than control patients. Given the chronicity of this patient group and the severity of their baseline depression and functional impairment, this improvement is encouraging. The higher level of nurse visits in the intervention group was expected, given the nature of the intervention. Both groups had very high levels of GP contact at baseline, which dropped slightly at follow-up, but were not significantly different between the two groups. Antidepressant usage dropped slightly in both groups over the follow-up period, but was significantly higher in the intervention group. There was no evidence that outcome varied by baseline diagnostic group.
Strengths and limitations
A particular strength was our large, nationally representative sample. The intervention was manualised, straightforward to implement and underwent successful piloting before the trial. Patients were rigorously assessed using standard diagnostic instruments, quality assurance for delivery of the intervention and outcome assessments was ensured and research masking maintained. The study was conducted across 42 UK general practices, but with fewer practices from deprived ethnically diverse inner city areas resulting in a low proportion of participants from Black and minority ethnic groups, so the results may be less applicable to these populations. Approximately 25% of patients initially approached attended and completed baseline interviews, which might be a limitation as regards generalisability, but analysis of our baseline data indicated that those participating were a severely affected and highly morbid group. Reference McMahon, Buszewicz, Griffin, Beecham, Bonin and Rost25 This was also reflected in their high rates of GP visits at baseline, which were nearly three times higher than general population figures. 26 There was some attrition over the trial period (65% completed 24-month assessments), although this is reasonable for this population and similar to other studies. Reference Rost, Nutting, Smith, Elliott and Dickinson10
In our pilot trial there were no identified issues of contamination. There was very little contact between the practice nurses and control patients, and where this occurred they were reviewed exclusively for physical health problems. There may have been a small risk of contamination in the main trial, which if present would lead to an underestimation of the effectiveness of the intervention.
Implications of these findings with reference to other studies
Our trial focused on the practice nurse as case manager within a chronic care model, with primary care support but, unlike US models of collaborative care, no input from specialist mental health services apart from for individual patients as part of their routine clinical care. This model is similar to that shown to be effective and in widespread use for other long-term conditions such as diabetes and chronic obstructive pulmonary disease, Reference Wagner, Austin and Von Korff27 and could be more easily implemented in a primary care setting using existing staff, such as practice nurses with no previous specific training in mental health. Practice nurses are available in many healthcare systems and achieve good results in managing other long-term conditions. Reference Bodenheimer, MacGregor and Stothart28 However, their training has been inadequate for working with people with mental health problems, Reference Crosland and Kai29 which was something we aimed to address with a focused, brief training course and clinical supervision over the study period.
A systematic review of RCTs of case management for depression in primary care highlighted a range of factors likely to be associated with a positive outcome, several of which were present in this trial. Reference Christensen, Griffiths, Gulliver, Clack, Kljakovic and Wells30 Systematic tracking of patients by a provider other than the doctor was significantly associated with improved depression outcomes and could be further improved by incorporating patient preferences into care, which were both factors we included. Practice nurses in our trial received brief training in simple problem-solving and motivational interviewing techniques. Reference Mynors-Wallis, Gath, Day and Baker15,Reference Rollnick, Heather and Bell16 Our qualitative evaluation indicated they used a problem-solving approach but made little use of motivational interviewing techniques in delivering the intervention. Reference Bennett, Walters, Drennan and Buszewicz31 They were encouraged not to consider themselves as therapists delivering a psychological intervention, but to refer patients to local psychological therapy services if indicated. However, they reported that access to psychological therapies was often not readily available for their patients, and their role in facilitating access to such treatments was therefore limited. Increased availability of appropriate, evidence-based psychological therapies might have improved patient outcomes.
Our results suggest improvements in functioning were greater than changes in symptoms of depression. This positive impact on functional impairment may be particularly important as there is evidence it is more significant in those with moderate to severe depression. Reference Mintz, Mintz, Arruda and Hwang32 Whereas functional impairment and disability associated with depression is often noted, there is relatively little emphasis on treatments that may positively have an impact on this. Reference Greer, Kurian and Trivedi33,Reference McKnight and Kashdan34 If participants engaged with the intervention and attended all the review sessions they had statistically significant improvements per session in both depressive symptoms and functional impairment. The two are likely to be linked and, although traditionally it is often considered that an improvement in mood leads to improved functioning, the converse may also be the case and it may be that in the context of chronic depression it may be possible to improve functioning without great improvements in depressive symptoms.
The absolute difference in functioning (WSAS) score in our study was modest, and its clinical significance is unclear. However, the results from our linked qualitative study gives support to some patients reporting meaningful changes in functioning resulting from the intervention. Reference Buszewicz, Griffin, Beecham, Bonin and Hutson35 Most participants reported an impact on some aspect of their lifestyle, with the potential impacts on diet, increasing exercise and sleep.
Implications for clinicians and policymakers
Systematic reviews of RCTs involving patients with depression in primary care or community settings have predominantly included acute cases. Reference Gilbody, Bower, Fletcher, Richards and Sutton11 Our population was more chronic and morbid and potentially more difficult to treat, Reference McMahon, Buszewicz, Griffin, Beecham, Bonin and Rost25 with very high baseline rates of GP consultations. Practice nurses are a widespread resource and in regular contact with such patients for their physical care, but often feel poorly skilled in working with mental health problems. Reference Crosland and Kai29 The training we provided was very well received Reference Bennett, Walters, Drennan and Buszewicz31 and we would encourage more widespread development of specific, and if possible more intensive, training courses for practice nurses in common mental health problems. We allowed the nurses to decide which approach to take with their patients with reference to the training they had received, but the training was of necessity brief and it would be interesting to see whether a more prescriptive approach to the management of these patients would give different results.
A difficult initial interaction with the nurse, patients who appeared to lack the motivation or time to attend appointments, were reluctant to discuss their difficulties or felt pessimistic that their situation might improve were all factors linked with poor attendance and such patients had poorer outcomes. Reference Bennett, Walters, Drennan and Buszewicz31 It may be appropriate for patients who do not engage well with the practice nurse as case manager to see someone with a mental health background in this role. Our trial suggests participants who engaged well and attended all sessions had more positive outcomes, irrespective of the severity or chronicity of their depression at baseline. We obtained useful information from our qualitative work, suggesting that early development of rapport with the practice nurse and motivation to change were important features of engagement. Reference Bennett, Walters, Drennan and Buszewicz31 This has implications for clinicians considering patient suitability for this type of service.
Our findings indicate that practice nurse-led enhanced care for chronic and recurrent depression shows promise for motivated patients from this highly morbid group in primary care. This model of care may have value in other healthcare systems with limited access to secondary care psychological or psychiatric services and should be evaluated in these settings.
In conclusion, patients with chronic or long-term depression are a neglected group as regards both clinical management and research into effective interventions. In our trial, although overall improvements in depressive symptoms were small and non-significant for patients receiving the intervention, there were significant improvements in work and social functioning. Further supplementary analysis indicated patients who regularly attended sessions over 2 years did well, with improvements in both depressive symptoms and functioning. In any implementation, it is key to identify patients more likely to engage with and benefit from such an intervention. The nurses' focus and approach on practical goals and problem-solving may have contributed to the improved levels of functioning obtained.
Acknowledgements
The authors would like to acknowledge and thank the Big Lottery as the funders of this research and the voluntary organisation Mind who were our collaborators. We would also like to thank the Medical Research Council General Practice Research Framework (MRC GPRF) nurses, participating practices and patients for their involvement, as well as the nurses, practices and patients from the four non-GPRF practices involved. We also received valuable support from the Mental Health Research Network (MHRN) and the Primary Care Research Network (PCRN). We are grateful to Professor Irwin Nazareth and Dr John Cape for their comments on an earlier draft of this paper.









eLetters
No eLetters have been published for this article.